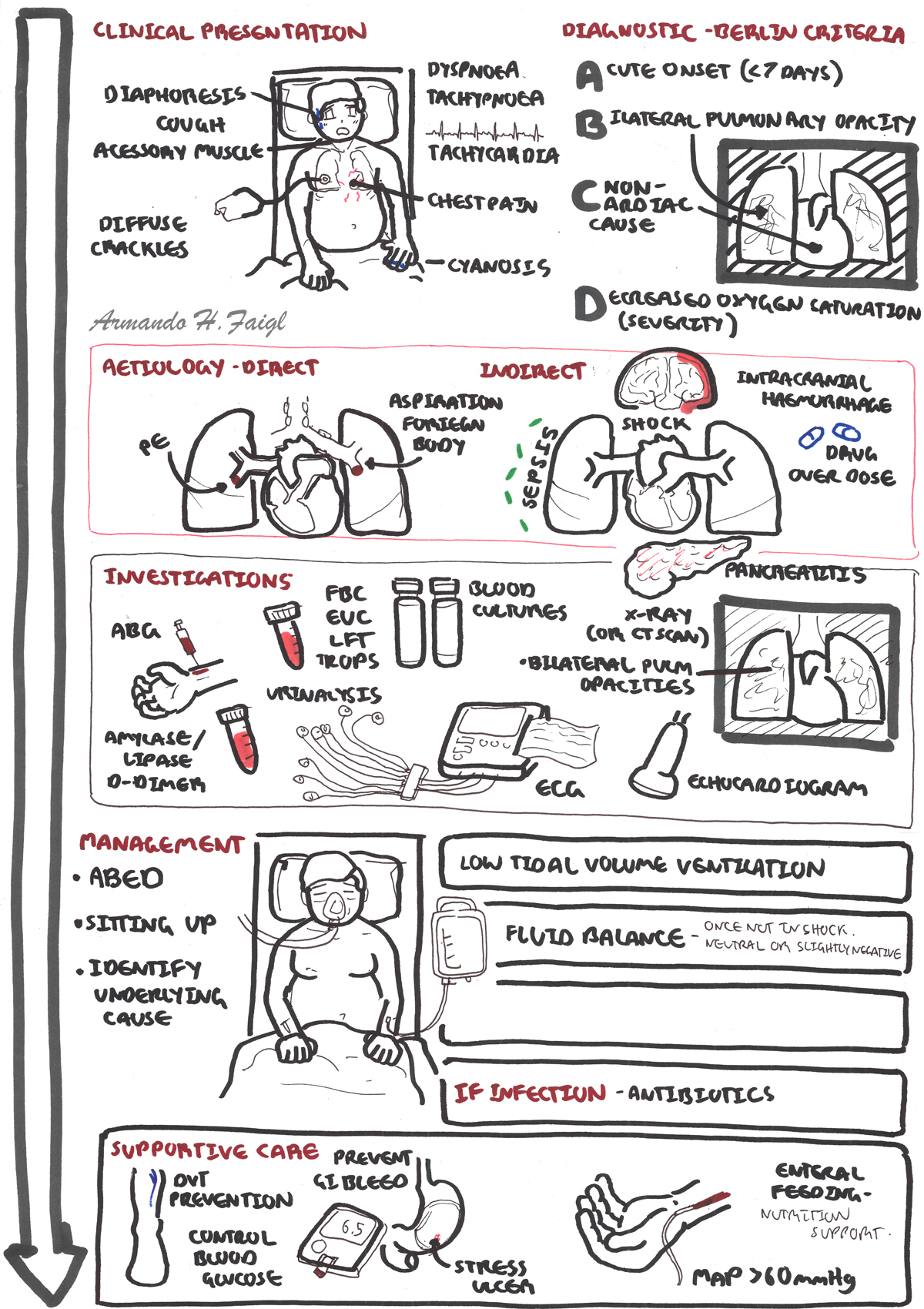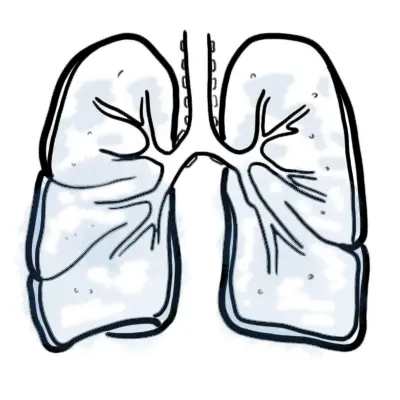
Overview ARDS is an acute, diffuse, inflammatory lung injury that leads to increased pulmonary vascular permeability, increased lung weight, and a loss of aerated tissue. Clinical hallmarks of ARDS are hypoxemia and bilateral radiographic opacities, while the pathological hallmark is diffuse alveolar damage.
Clinical Presentation
| Remember Clinical hallmarks of ARDS are hypoxemia and bilateral radiographic opacities, while the pathological hallmark is diffuse alveolar damage. |
Clinical Course
Diagnostic Criteria – Berlin Definition
Aetiology
Pathophysiology
| Side note Mortality is 30-40% and mostly from extra-pulmonary complications |
Complications of ARDS