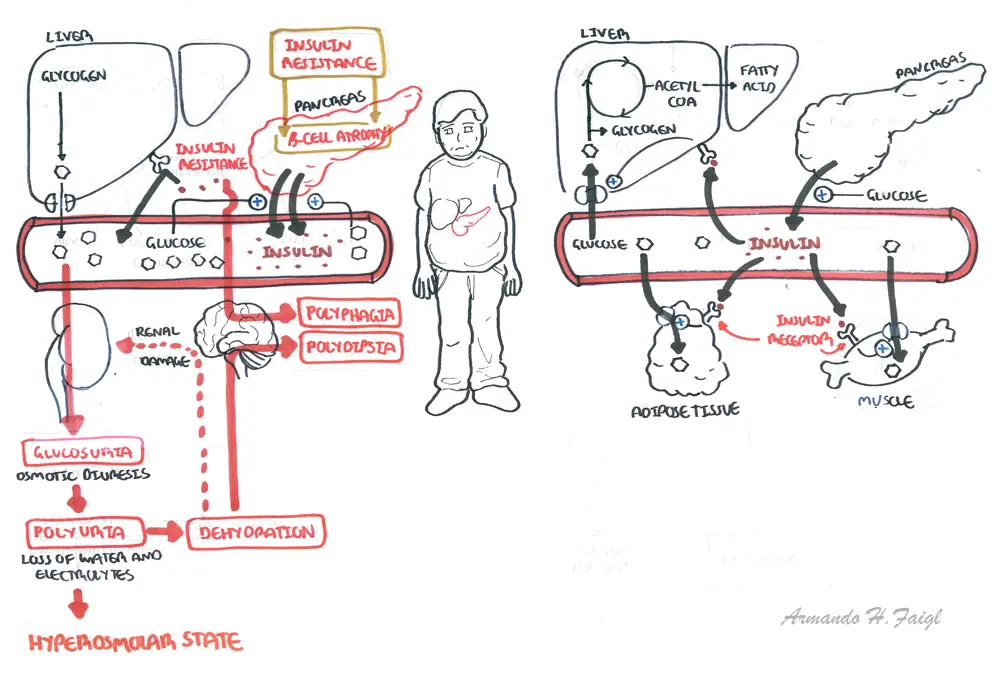
Overview Diabetes Mellitus type II is a progressive disorder defined by deficits in insulin secretion and action (insulin resistance). 1 in 12 people have diabetes (50% do not know they have it). Diabetes type II accounts for over 90% of all diabetes cases. The remaining 10% include type I diabetes. People with type II diabetes are often asymptomatic initially, and may not be recognised for many years. Type II is not usually associated with DKA and insulin is not essential for survival but is often required to achieve adequate glycemic control.
| Definition Diabetes: A group of metabolic diseases in which there are high blood sugar levels over a prolonged period. Diabetes Mellitus Type I: Autoimmune destruction of beta cells in the pancreas Diabetes Mellitus Type II: Insulin resistance followed by beta cell atrophy Gestational Diabetes: diabetes diagnosed during the second half of pregnancy with no prior existing diabetes. |
The pancreas sits in the upper abdomen behind the stomach. The pancreas consists of the following parts:
The head is encircled by duodenum and tail in contact with spleen. The pancreas has a poorly developed capsule & therefore adjacent structures (common bile duct, duodenum, splenic vein, transverse colon) are commonly involved in inflammatory process. It is an exocrine and endocrine organ.
Blood Supply
Venous drainage
Nerve invervation
Lymphatic drainage
Embryology
Exocrine glands bundle up to form the pancreatic acinar which secrete digestive enzymes into the pancreatic duct which makes its way to the ampulla of vater and into the duodenum. The pancreatic duct joins with the common cystic duct. There is the main pancreatic duct and an accessory pancreatic duct which does not join with the common cystic duct so when obstruction occurs due to gallstones, the pancreas is still able to secrete its enzymes into the duodenum. Pancreatic enzymes include:
The endocrine cells make up the islets of Langerhan in the pancreas. The Islet of Langerhan make up 2% of the pancreas. There are many endocrine cells:
The Beta cells produce insulin. The beta cells make up the majority of endocrine cells in the pancreas. Beta cells are stimulated when blood glucose is high. Once insulin is secreted it targets many organs especially the liver to promote glucose storage as glycogen and lipids.
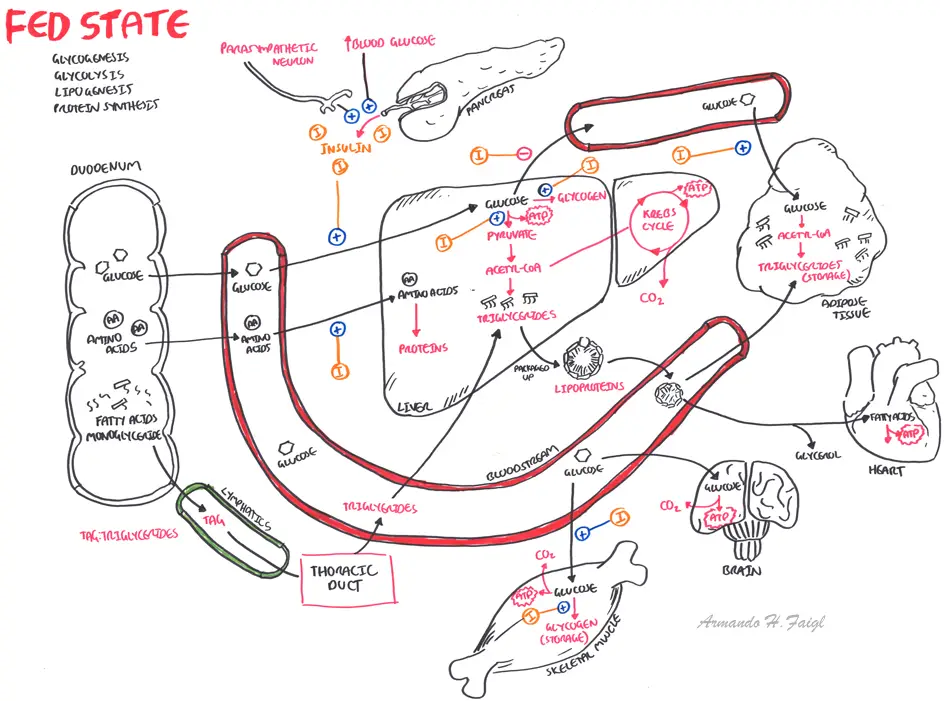
Normal physiology of what happens after you eat. Insulin plays a major role in the bodies response to feeding. Insulin promotes storage of nutrients. Insulin dysfunction results in elevated glucose levels and distributes homeostasis.
| Watch the video: Fed State |
Diabetes in General
Diabetic Complications (advanced disease)
Diabetic Retinopathy
Diabetic Neuropathy
Diabetic Nephropathy
More info on the Long-Term Complications of Diabetes
| Side Note Plasma Fructoseamine is an alternative to HbA1c. It correlates with blood glucose levels and has a shorter half. It is a superior marker to HbA1c in pregnancy, in assessing the effect of medication on diabetes, in diseases that affect erythrocyte number (ex. Sickle cell, hemolytic anaemia). |
Diabetes case detection
Diagnosis (7/11 rule)
*There is no definitive diagnostic criteria for Diabetes. The criteria varies between countries
| Remember 7/11 rule. 7 at fasting. 11 after eating. |
Differential Diagnosis for Diabetes Type II
| Gestational Diabetes is defined as glucose intolerance resulting in hyperglycemia of variable severity, with onset or first recognition during pregnancy |
| Diabetes Type I is cause primarily by immune-mediated destruction of the insulin-producing beta-cells. Islet cell antibodies and antibodies to insulin, glutamic acid decarboxylase and the tyrosine phosphatase. This form of diabetes is usually rapid in onset and within five year the person usually has an absolute deficiency in insulin requiring lifelong treatment with insulin, otherwise they risk developing DKA. |
Differential Diagnosis for Diabetic Complications
Differential Diagnosis for Diabetic Retinopathy
Differential Diagnosis for Diabetic Neuropathy
| Guillain-Barré syndrome is a disorder in which the body's immune system attacks part of the peripheral nervous system. Its like multiple sclerosis but it effects the peripheral nervous system. |
Differential Diagnosis for Diabetic Nephropathy
| Watch the video: Diabetes Pathophysiology |
| Watch the video: Pathophysiology of Diabetic complications |
Management priorities for diabetes are
General Management
| Side Note Red blood cells contain haemoglobin HbA. Glucose bind to haemoglobin making glycosylated haemoglobin HbA1c. Once haemoglobin is glycosylated it stays this way until the red blood cell dies. Red blood cells have a turn around of 120days. Therefore monitoring HbA1c can give an estimate of blood glucose control. If the HbA1c is low it means the glucose level has been low for the 120day period - which means diabetes is under control. |
| Watch Pharmacology of Diabetes Mellitus Type II |
| Indications for Insulin |
| Acute metabolic complications |
| Perioperative in patients undergoing surgery |
| Severe infection |
| Pregnancy and lactation |
| Fasting plasma glucose >300mg/d |
| Failure of oral anti-diabetic agent/contraindication of oral anti-diabetic agents |
Screening for Diabetic Complications
Microvascular Complications
Macrovascular Complications
More info on the Long-term Complications of Diabetes
Other complications
| Remember glucose of 4 hits the floor (hypoglycemic) |
Prognosis
| DIFFERENCES BETWEEN TYPE I AND TYPE II | ||
| Type I | Type II | |
| Epidemiology | Often starts before puberty | Older patients |
| Morphology | Usually lean | Usually overweight |
| Genetics | HLA D3 and D4 | No HLA association |
| Cause | Autoimmune β cell destruction | Insulin resistance/β cell dysfunction |
| Presentation | Polydipsia, polyuria, weight loss, ketosis (can present with DKA) | Asymptomatic. Complications associated with diabetes |
| Complications | DKA | HHS |
