
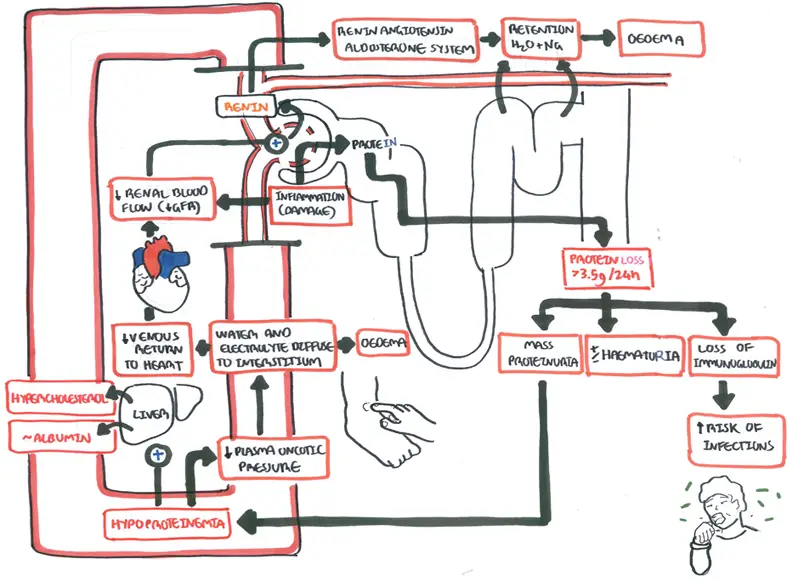
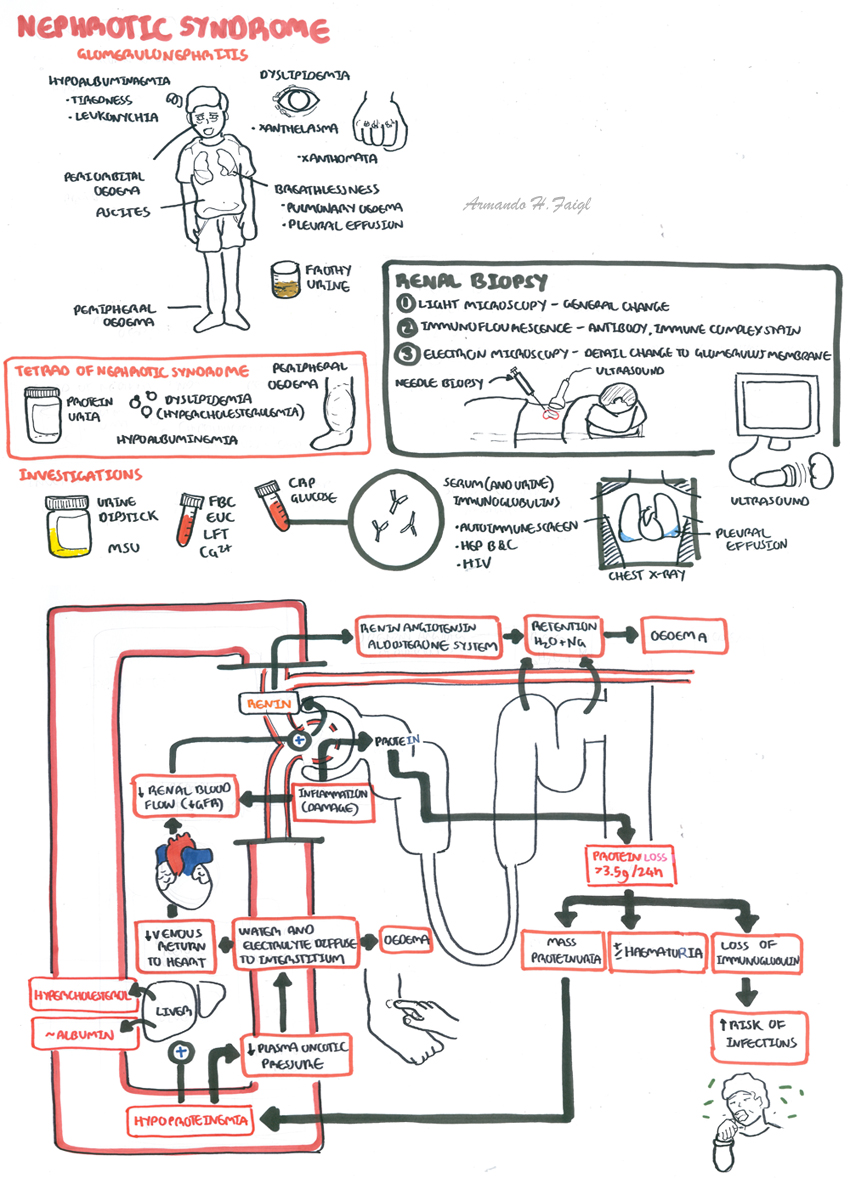
Overview Nephrotic syndrome is a relatively rare but important manifestation of kidney disease. Nephrotic syndrome classically presents with heavy proteinuria, minimal hematuria, hypoalbuminemia, hypercholesterolemia, edema, and hypertension. In general, all patients with hypercholesterolemia secondary to nephrotic syndrome should be treated with lipid-lowering agents because they are at increased risk for cardiovascular disease. Nephrotic syndrome has serious complications and must be part of the differential diagnosis for any patient presenting with new onset edema. All patients should be referred to a nephrologist for further investigation, which often include a renal biopsy.
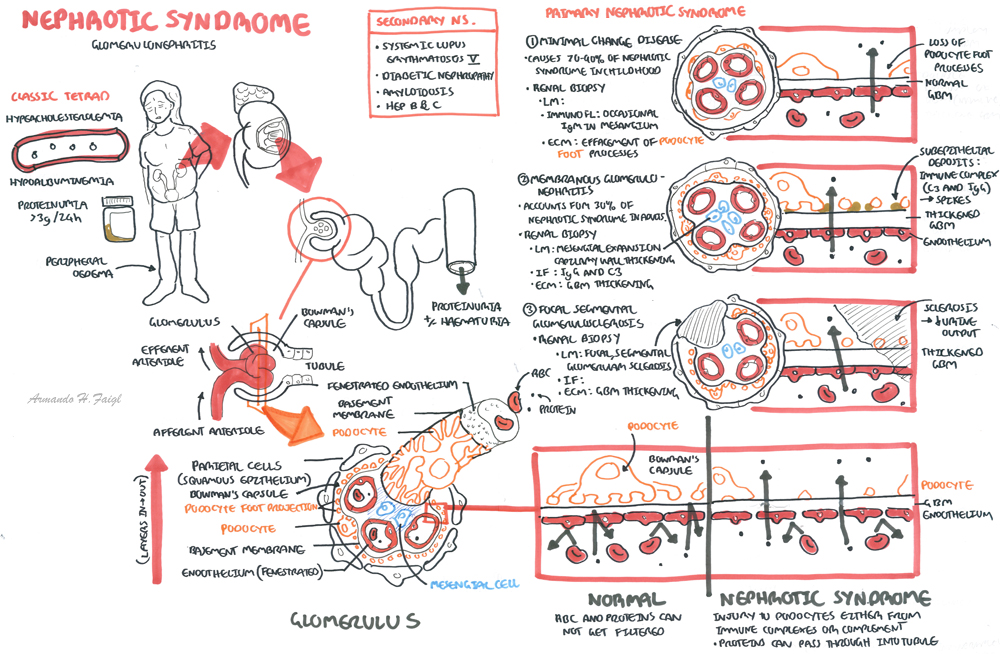
| Remember Classic tetrad of Nephrotic syndrome is proteinuria (>3g/24hr), hypoalbuminemia, hypercholesterolemia an oedema. |
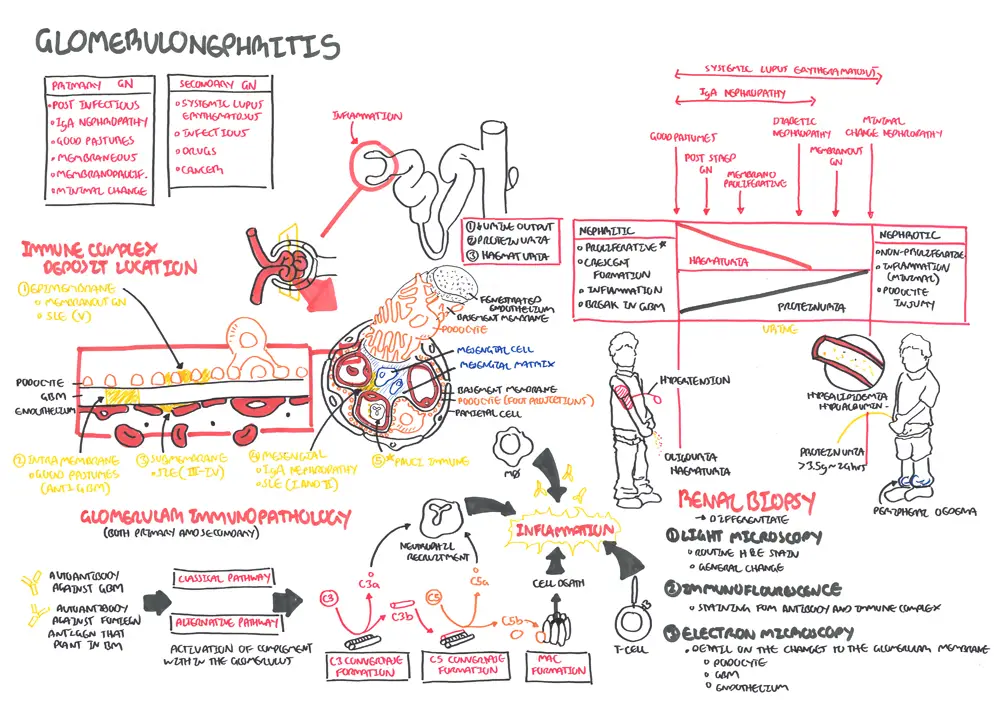
Glomerulonephritis is inflammation of the glomerulus. There are two broad types Nephritic glomerulonephritis and nephrotic glormerulonephritis
Remember Glomerulonephritis is divided into two broad groups:
|
Nephrotic Syndrome
The page will focus on four common nephrotic syndromes towards the end:
| Side note Most common cause of chronic kidney disease and nephrotic syndrome is Diabetic nephropathy |
The kidneys are retroperitoneal organs (at the back of abdomen) and lies between T11 and L3, the left kidney lying slightly higher than the right kidney.
The kidney is surrounding by an outer membrane called the renal capsule. The outer layer of the kidney is the renal cortex where most of the nephrons are situated. The inner layer is the renal medulla which contain renal pyramids. The renal pyramids drain urine into the minor - major calyces before draining to the renal pelvis then the ureter.
Arterial blood supply
The Nephrons are the functional units of the kidney. There are millions. The nephron is made up of:
The glomerulus is a network of blood vessels that are located within the bowman's capsule. To understand the cause, pathophyiology and effect of glomerulonephritis it is important to learn the layers of the glomerulus + bowman's capsule
From inside out the layers are:
Clinical Presentation
Examination
Oedema
Hypoalbuminemia
Dyslipidemia
Breathlessness with chest pain (Pulmonary Oedema and pleural effusion)
Frothy Urine
This section will mainly focus on the Primary Aetiology + Diabetic Nephropathy
Primary Aetiology of Nephrotic Syndrome
Secondary Aetiology Nephrotic Syndrome
Other causes of bilateral swollen legs (because one of the classic presentations of nephrotic syndrome is oedema)
General
Check for other systemic diseases and causes of nephrotic syndrome
Chest Xray - if breathless (effusion)
Abdominal or renal ultrasound
Renal biopsy to perform microscopy, immunofluorescence and Electromicrography
Nephrotic Glomerulonephritis is a renal condition affecting the podocytes. This causes a leaky glomeruli leading to proteinuria and subsequent hyperlipidemia, hypoalbuminemia and oedema
Pathophysiology - General
Overview Minimal change disease (MCD), sometimes known as nil lesion, causes 70–90% of nephrotic syndrome in childhood but only 10–15% of nephrotic syndrome in adults. Minimal change disease usually presents as a primary renal disease but can be associated with several other conditions, including Hodgkin’s disease, allergies, or use of nonsteroidal anti-inflammatory agents.
Clinical Presentation
| Minimal Change Disease The most common presentation of MCNS is oedema. MCNS is characterised by oedema, selective proteinuria, hypoalbuminaeia, hypercholesterolaemia, and a normal glomerular filtration rate. Renal Biopsy: The only abnormality is diffuse effacement and fusion of epithelial cell fot processes. |
Renal Biopsy
Management
| Side note After initial treatment, proteinuria <0.3 g/day is defined as complete remission; a reduction of baseline proteinuria by >50% with a final value <3 g/day is defined as partial remission. |
| Remember 90% 0f patients experience a frequently relapsing or steroid-dependent course with steroid toxicity. These patients are candidates for treatment with second line drugs - cyclophosphamide or tacrolimus |
Complications
| Side note Relapses occur in 70–75% of children after the first remission, and early relapse predicts multiple subsequent relapses |
Focal segmental glomerulosclerosis (FSGS) refers to a pattern of renal injury characterised by segmental glomerular scars that involve some but not all glomeruli; the clinical findings of FSGS largely manifest as proteinuria. When the secondary causes of FSGS are eliminated, the remaining patients are considered to have primary FSGS.
| Side note The incidence of this disease is increasing, and it now represents up to one-third of cases of nephrotic syndrome in adults |
Renal Biopsy
Management
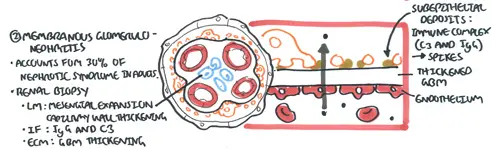
Membranous glomerulonephritis (MGN), or membranous nephropathy, accounts for approximately 30% of cases of nephrotic syndrome in adults, with a peak incidence between the ages of 30 and 50 years and a male to female ratio of 2:1.
| Remember Membranous glomerulonephritisis is rare in childhood and the most common cause of nephrotic syndrome in the elderly |
Renal Biopsy
Overview Type II Diabetes Mellitus is the leading cause of Chronic Kidney Disease. It is classified as a secondary nephrotic syndrome. ~10% have nephropathy at diagnosis and up to half will go on to develop it over the next 20yrs. 20% of people with Type II diabetes will develop end stage kidney disease. Everyone with Diabetes should be screened yearly for microalbuminuria.
Clinical features - Nephrotic Syndrome with signs and symptoms of diabetes (hyperglycemia)
Pathological features Diabetic nephropathy is defined by characteristic structural and functional changes. The predominant structural changes include
| Staging | |
| Class I | Isolated glomerular basement membrane thickening. There is no evidence of mesangial expansion, increased mesangial matrix, or global glomerulosclerosis involving >50 percent of glomeruli. |
| Class II | Mild (class IIa) or severe (class IIb) mesangial expansion. |
| Class III | At least one Kimmelstiel-Wilson lesion (nodular intercapillary glomerulosclerosis) is observed on biopsy and there is <50 percent global glomerulosclerosis. |
| Class IV | Advanced diabetic sclerosis. There is >50 percent global glomerulosclerosis. |
Management and Prognosis Microalbuminuria is reversible if caught early and managed vigorously.
More info on Chronic Kidney Disease
Complications
| Watch Video Nephrotic Syndrome - Overview |
| Watch Video Nephrotic Syndrome Types |
