Overview Asthma is a chronic airway inflammation disorder due to complex interactions between inflammatory cells, mediators and airway cells. In young children in whom lung function testing is not feasible, including most preschool children, asthma is defined by the presence of variable respiratory symptoms. Asthma is one of the most common causes of presentation to the Emergency department It implies reversible airway constriction (peak flows vary by >20%) +/- wheeze, dyspnoea or cough
| Definition Asthma: Condition of bronchial hyperactivity and smooth muscle hypertrophy leading to a chronic inflammatory condition of the airways associated with widespread bronchospasm that is reversible. Acute cough: Condition for less than 3 weeks, most commonly caused by acute upper respiratory infection but also may be caused by congestive heart failure, pneumonia, and pulmonary embolism. Chronic cough: Condition for longer than 3 to 8 weeks (case definitions vary). Smoker - chronic obstructive pulmonary disease. Nonsmoker with a normal chest radiograph and not taking an ACE inhibitor, it may be due to postnasal drip, gastroesophageal reflux disease (GERD), or asthma. |
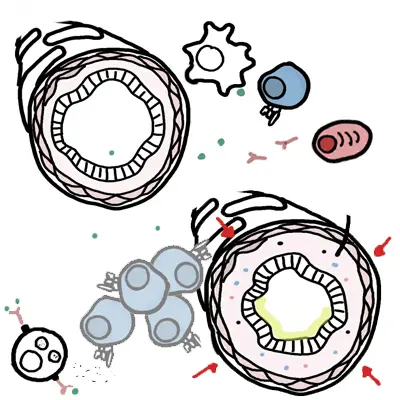
Airway obstruction occurs due to a combination of:
This page will mainly focus on paediatric asthma
Epidemiology
Infrequent intermittent asthma (70-75% of cases)
Frequent intermittent asthma (20-25% of cases)
Persistent asthma (5-10% of cases)
| Asthma Triad CDE: Cough, Dyspnea, Expiratory wheeze |
Parental anxiety should not be discounted: it is often of significance even if the child appears relatively well.
Certain thing can trigger a wheezing episode in asthma
Side note Spirometry
|
Diagnosis
Aetiology
Pathophysiology
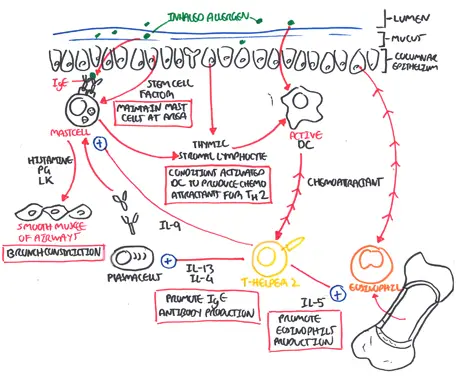
| Watch Asthma Pathophysiology |
Asthma action plan
The essential elements of asthma self-management education are:
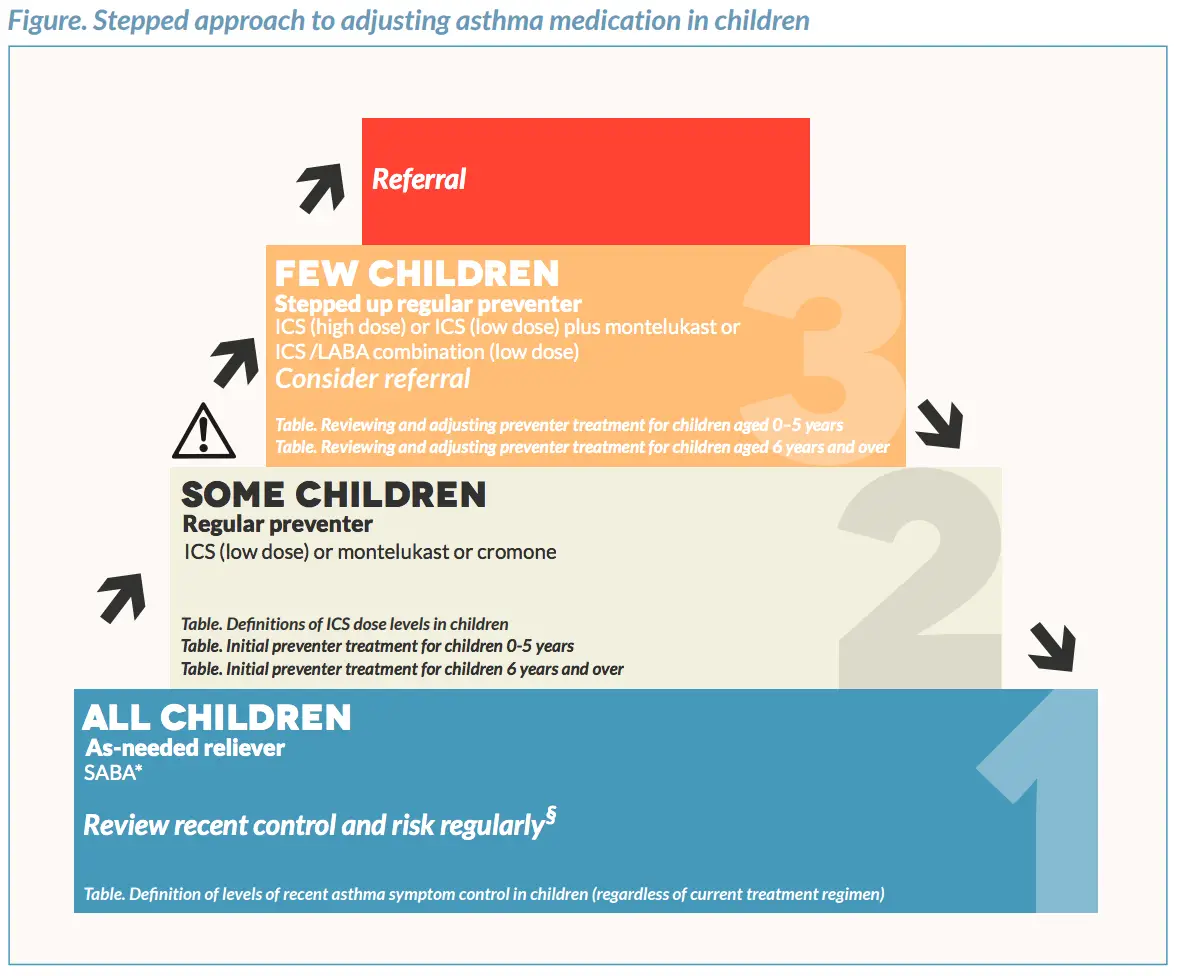
Image from Australian Asthma Handbook
| MEDICATIONS FOR CHILDHOOD ASTHMA | |||
| Medication | Mechanism of Action | Contraindication | Side-effects |
| Short Acting b2-agonist | Sympathomimetic relaxes bronchial smooth muscles by stimulating B2 receptors | Tremors, palpitations, headache. Hyperglycaemia, tachycardia, muscle cramps, lactic acidosis, hypokalaemia | |
| Long Acting b2-agonist | Sympathomimetic relaxes bronchial smooth muscles by stimulating B2 receptors | Tremors, palpitations, headache. Hyperglycaemia, tachycardia, muscle cramps, lactic acidosis, hypokalaemia | |
| Ipratropium bromide | Anticholinergic M3 receptor antagonist – promote bronchodilatation by inhibiting parasympathetic bronchomotor tone | Dry mouth, throat irritation, blurred vision, dizziness, urinary retention, constipation | |
| Theophilines (aminophylline) |
Not understood – thought to have adrenergic effects as well as anti-inflammatory effects | Nausea, vomiting, diarrhoea, GOR, anxiety, tremor, palpitations, seizures, arrhythmias, tachycardia | |
| Corticosteroids | Reduce airway inflammation and bronchial hyper-reactivity | Candidiasis, bruising, facial skin irritation due to nebules, systemic effects (adrenal suppression, bone density loss, glaucoma, skin thinning and bruising, impaired growth) | |
| Magnesium | |||
| Adrenaline | |||
Assessment of and management of Asthma in Emergency
