Overview Third most common cause of death worldwide and most common cause of neurological disability. It is subdivided into ischaemic stroke (caused by vascular occlusion or stenosis) and haemorrhagic stroke (caused by vascular rupture, resulting in intra-parenchymal and/or subarachnoid haemorrhage).
| Defintion Stroke: Acute onset of a focal neurologic deficit due to a cerebral infarction or hemorrhage. Transient Ischaemic Attack (TIA): Transient episode of neurological dysfunction caused by focal brain or retinal ischaemia, without infarction. When there is evidence of brain infarction, the episode is considered to be a mild stroke (if symptoms are minor or disappear). Amaurosis Fugax: Transient monocular blindness that often is described as a gray shade being pulled down over the eye caused by ischemia to the retinal artery. |
Non-Modiafiable Risk Factors
Modifiable risk factors
In Women
| Remember The highest- risk patients for stroke are those with previous ischemic events such as TIA |
Types of stroke
| Anatomical classification - Oxford territorial classification |
| Total anterior circulation infarct |
| Partial anterior circulation infarct |
| Posterior circulation infarct |
| Lacunar infarct |
| Pathophysiological classification - TOAST |
| Large-artery atherosclerosis (embolus/thrombosis) |
Cardioembolism (high-risk/medium-risk)
|
| Small-vessel occlusion (lacune) |
Stroke of determined aetiology
|
| Stroke of undertermined aetiology |
| Think cardioembolism can cause multiple infarcts, often in different vascular territories. Whereas large artery atherosclerosis is a single area of infarct. |
Cerebral anatomy and blood supply
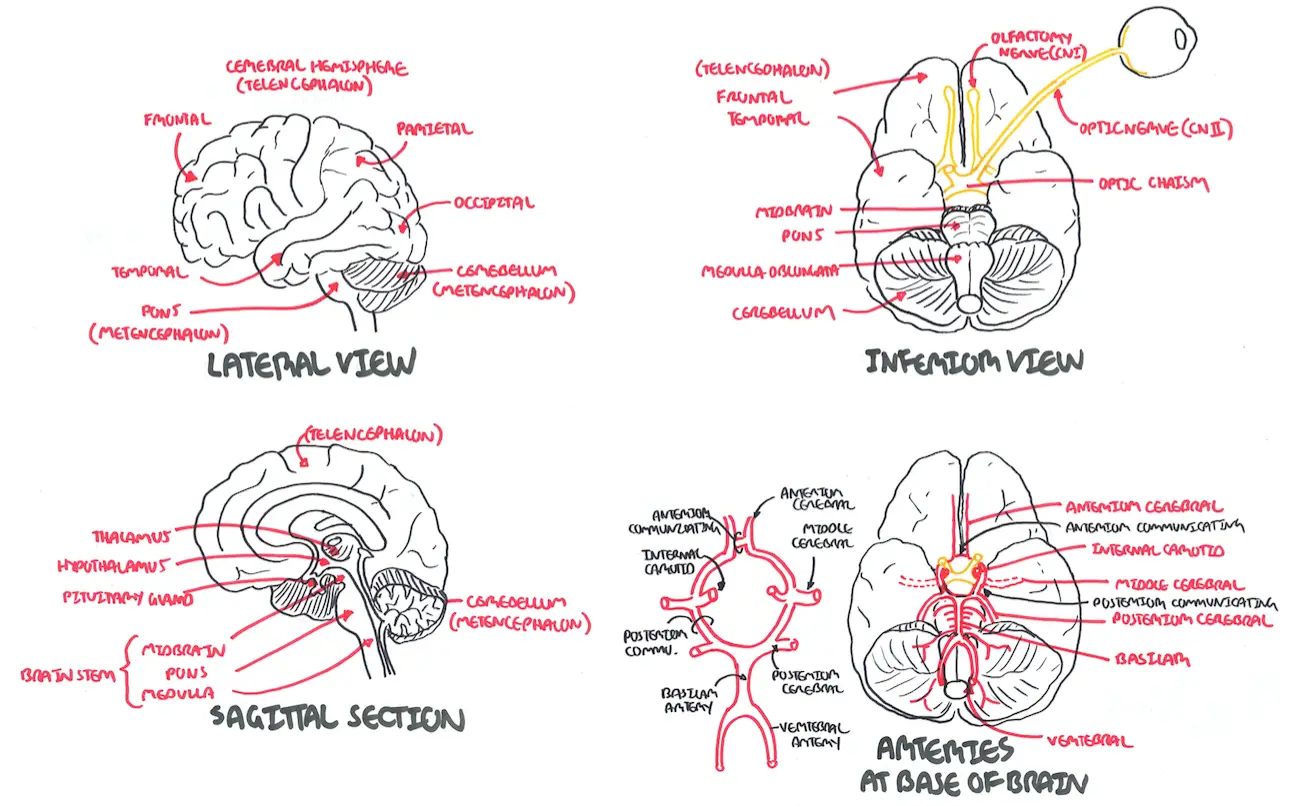
| Watch Anatomy - Cerebral anatomy and blood supply (Circle of Willis) |
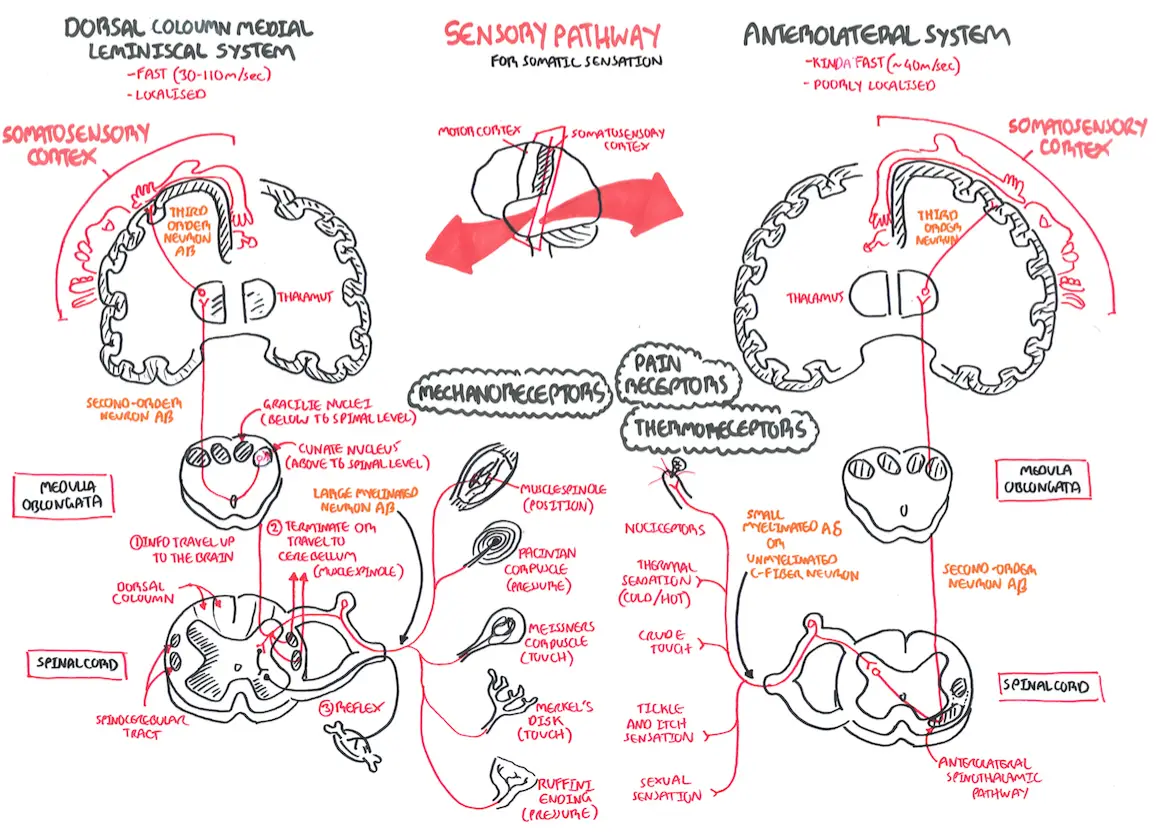
Sensory Pathways
Motor Pathways
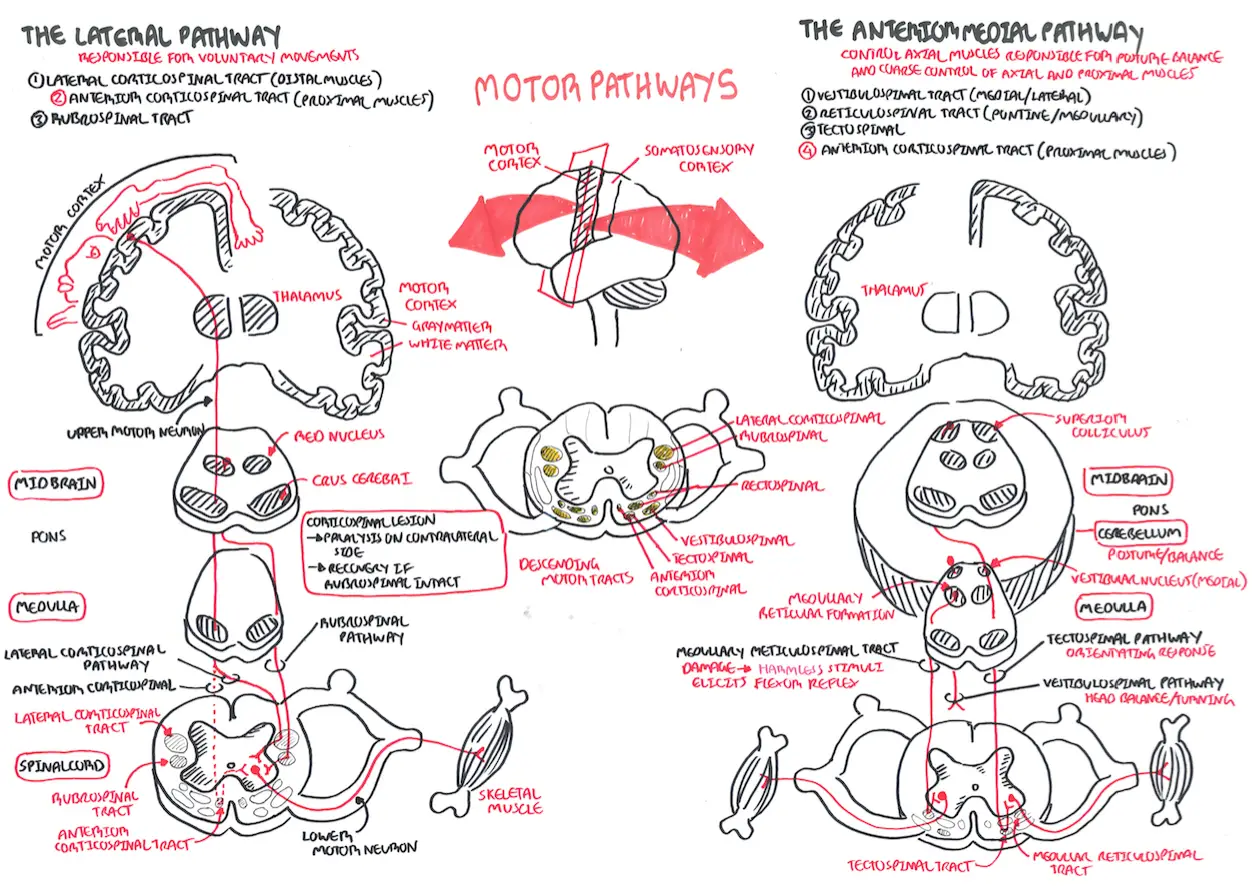
| Watch Motor Pathway |
| Rememeber FAST - acute signs and symptoms of stroke Face: unilateral drooping Arms: these may feel weak and numb. Patient may not be able to lift them Speech: slurring of speech Time: time for emergency medical attention |
Symptoms
Signs
Clinical Presentation based on location of "stroke" using the Anatomical classification - Oxford territorial classification:
| Anterior circulation (carotid territory) |
| Amaurosis fugax/retinal infarction. |
| Hemiparesis |
| Hemisensory loss |
| Hemianopia (optic tract and radiation) |
| Dysphasia |
| Sensory inattention |
| Visual inattention |
| Posterior circulation (vertebrobasilar) |
| Ataxia |
Cranial nerve involvement:
|
| Hemiparesis (may be bilateral) |
| Hemisensory loss (may be bilateral) |
| Hemianopia (occipital lobe) |
| Cortical blindness—basilar artery occlusion |
| Lacunar |
| Pure motor strokes (face, arm, and leg) in the posterior limb of internal capsule |
| Pure sensory stroke (thalamus) |
| Ataxic hemiparesis (weakness and ataxia affecting the same side) due to a pontine lesion |
| Clumsy hand/dysarthria due to a lesion in the pons or in its internal capsule. |
Imaging
Infarcts best detected by MRI (but not in first few hours) > CT
| Remember Imaging should be performed within 24 hours to exclude haemorrhagic stroke and other causes, e.g. tumours. |
General
Other blood investigations to consider
Other investigation
| CONDITION | CLINICAL MANIFESTATION |
| Brain tumor | Severe unilateral headache with nausea and vomiting |
| Central nervous system infection (e.g., meningitis, encephalitis) | Fever, headache, confusion, neck stiffness, nausea, vomiting, photophobia, change in mental status |
| Falls/trauma | Headache, confusion, bruising |
| Hypoglycemia | Confusion, weakness, diaphoresis |
| Migraines | Severe headaches with or without photophobia, younger age |
| Multiple sclerosis | Diplopia, limb weakness, paresthesia, urinary retention, optic neuritis |
| Seizure | Confusion with or without loss of consciousness, urinary incontinence, tongue biting, tonic-clonic movements |
| Subarachnoid hemorrhage | Severe headache with sudden onset and photophobia |
| Vertigo (central or peripheral) | Generalized dizziness and diaphoresis with or without hearing loss |
| Remember TIA is more likely with sudden onset, unilateral paresis, speech disturbance, or transient monocular blindness. |
The development of an acute stroke or transient ischaemic attack is a medical emergency.
| INDICATION FOR CT/MRI |
| Patient on anticoagulants or with abnormal coagulation |
| Plan to give thrombolysis or immediate anticoagulants |
| Deteriorating conscious level or rapidly progressing deficits |
| Suspected cerebellar haematoma, to exclude hydrocephalus |
General management
| Remember Urgent brain imaging is required. Computerised tomography (CT) can help to exclude a stroke mimic and to differentiate haemorrhagic to ichaemic stroke |
Acute ischaemic stroke
| Pharmacology Alteplase is a recombinant tissue plasminogen activator |
| Side note Eligible stable patients should undergo carotid endarterectomy as soon as possible after the stroke event (ideally within two weeks). |
Acute Haemorrhagic Stroke
| Remember Some patients with an intracerebral haemorrhage will be on warfarin therapy. Warfarin therapy must be urgently reversed with a combination of prothrombin complex concentrate, fresh frozen plasma and vitamin K. |
Complications
Prognosis Ischaemic Stroke
Prognosis Haemorrhagic Stroke
