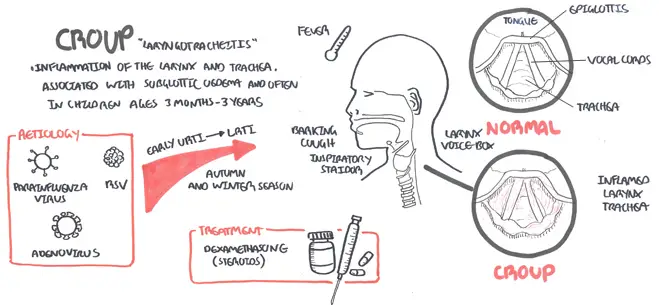
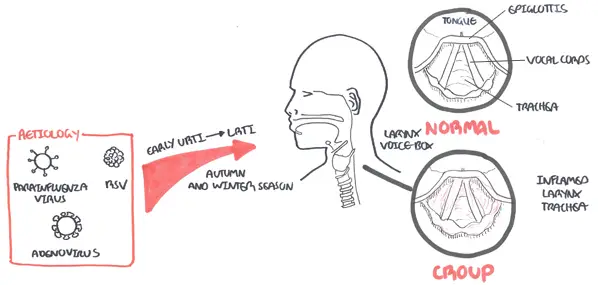
Overview Croup, also known as largnotracheobronchitis, is a usually self limiting upper airway viral infection causing upper airway obstruction. Croup is more common in boys than in girls, usually occurs between six and 36 months of age, and peaks during the second year of life. Croup is usually caused by viruses, which are detected in up to 80 percent of patients (parainfluenza the most common).
Croup is the clinical syndrome of:
| Definition Croup: a viral infection which causes swelling of the voice box (larynx) and windpipe (trachea). Spasmodic Croup (laryngismus stridulus): a noninfectious variant of the disorder, with a clinical presentation similar to that of the acute disease but with less coryza. This type of croup always occurs at night and has the hallmark of reoccurring in children Stridor: caused by partial upper airway obstruction and is typically heard in inspiration, although it can also be heard on expiration if the obstruction is below the larynx |
| Remember Croup symptoms usually start with flu like symptoms. Croup is caused by viruses, with para-influenza virus (types 1 to 3) as the most common |
Typically, viral croup develops over days with a upper respiratory tract infection, with low-grade fever and coryza followed by a barking cough and various degrees of respiratory distress. In most children, the symptoms subside quickly with resolution of the cough within two days.
| Classic Tetrad: barking cough, stridor, hoarse voice, and respiratory distress |
| Think Children with croup should have minimal examination. Do not examine throat. Do not upset child further. |
Differentials for stridor
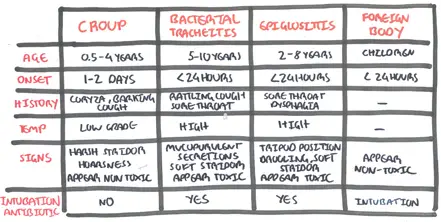
Table of difference between the common causes of stridor in infants
| Remember Children six to 36 months of age who present with abrupt onset of barking cough, hoarseness, and inspiratory stridor likely have croup. |
Other Differential
Three factors to consider when deciding whether the presence of stridor and respiratory accessory muscle use relate to croup or another disease.
1. Age of child
2. Character is stridor
3. Toxicity of child
Croup is a clinical diagnosis based on early respiratory infections followed by a barking cough
| Side Note Investigations including Nasopharyngeal Aspirate, Chest X-Ray, blood tests are NOT usually indicated and may cause the child distress and worsening of symptoms |

The classic steeple sign (arrow) of croup on radiograph
Mild Airway Obstruction
Moderate Airway Obstruction
Severe Airway Obstruction
Soft stridor, irritability, tachycardia, pallor indicates imminent airway obstruction
A single dose of dexamethasone is recommended in all patients with croup, including those with mild disease. Nebulized epinephrine is an accepted treatment in patients with moderate to severe croup.
Mild Airway Obstruction
Moderate Airway Obstruction
Severe Airway Obstruction
| Remember Antibiotics have no role in uncomplicated croup as it has a viral aetiology |
| Pharmacology Corticosteroids benefits patients with croup presumably by decreasing edema in the laryngeal mucosa, and is usually effective within six hours of treatment. Corticosteroid therapy decreases the need for additional medical care, hospital stays, and intubation rates and duration. No adverse effects have been associated with appropriate corticosteroid therapy in patients with croup. The risks of single-dose corticosteroids are very low |
Complication Croup is a benign condition with a low mortality rate
Typically, viral croup develops over days with a upper respiratory tract infection, with low-grade fever and coryza followed by a barking cough and various degrees of respiratory distress. In most children, the symptoms subside quickly with resolution of the cough within two days.
Conversely, spasmodic croup is said to be more in atopic, older children. Spasmodic croup comes on rapidly overnight in children who were perfectly well when they went to sleep. Spasmodic croup often runs a shorter course.
|
CONDITION |
HISTORY |
EXAMINATION |
WORK UP |
AETIOLOGY |
|
Laryngotracheitis (croup) |
Barking cough, coryza |
Low-grade fever, nasal flaring, respiratory retractions, stridor |
Generally not indicated |
Parainfluenza virus types 1 to 3, influenza, respiratory syncytial virus |
|
Spasmodic croup (recurrent croup) |
Usually recurrent, short duration, barking cough |
Afebrile, less retractions and nasal flaring |
Generally not indicated, but bronchoscopy (especially in children younger than three years) and endoscopy may be considered |
Same as viral croup, with possible allergic component or gastroesophageal reflux |