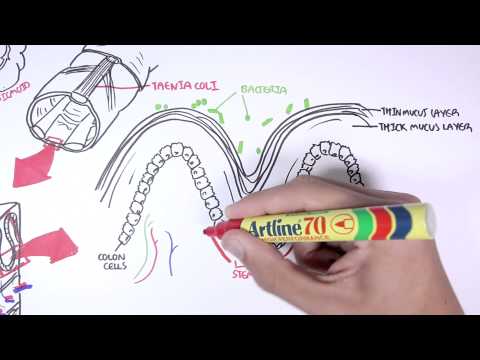
0:00 Hello, in this video we're going to talk about anorectal abscess. 0:08 This is an overview, an introduction. 0:13 Now anorectal abscess is localized infection with a collection of pus in the an 0:18 orectal 0:19 area. 0:21 And the abscess is usually a result from invasion of normal rectal flora, so 0:25 the normal microbes 0:27 in anorectal area causes anorectal abscess. 0:33 Let us now compare a normal to anorectal abscess. 0:36 Let's look at the normal anatomy first. 0:40 So here we have the anus, the rectum, the anal canal. 0:45 The anal canal has actually involuntary muscles, the internal anal sphincters, 0:51 and it also has 0:51 the voluntary muscles, the external anal sphincter. 0:56 The levato ni, also known as the muscular pelvic diaphragm, is the muscle 1:03 tenderness 1:04 sheath that forms the majority of the pelvic floor. 1:09 And it supports the pelvic visceride, it aids in urinary and fecal movement, as 1:16 well 1:16 as maintaining continents. 1:20 The peritoneum that lines the abdominal cavity also lines the digestive organs 1:28 itself, including 1:30 the rectum. 1:32 An important anatomical site to know is the pectinate line, also known as a 1:37 dentate line. 1:39 Now the pectinate line is a clinically important landmark due to the fact that 1:44 it is visible 1:45 and approximates the level of certain anatomical changes. 1:49 So what are these changes? 1:53 Well embryologically speaking, above the pectinate line is where there are 2:00 cells from an embryological 2:03 endoderm origin, and below the pectinate line is the ectoderm in origin. 2:12 This is different because the endoderm means it is part of the abdominal organs 2:18 essentially, 2:18 and the ectoderm means it is the skin. 2:21 And because below the pectinate line it is ectoderm in origin, so skin 2:27 essentially, it 2:28 is very sensitive. 2:30 So below the pectinate line it is a very sensitive area, and pain that occurs 2:34 here is very painful 2:36 and well localized. 2:39 Going back to the peritoneum here, again the peritoneum is the lining of the 2:43 internal abdominal 2:44 cavity and also essentially covers or coats the digestive organs, so the rectum 2:53 and other 2:54 remaining colon is within the abdominal cavity and so has a visceral peritoneum 2:59 around them. 3:01 Now let us look at the anorectal abscess. 3:03 They can occur in many areas around what we have drawn. 3:07 They can be deep or they can be superficial, depending on where the abscess 3:13 occurs. 3:14 The abscess is referred to or called different things. 3:18 So for example, the abscess that is formed between the internal and external sp 3:23 hincta 3:23 are called the intersphinteric abscess. 3:27 Abscess just below the skin and confined to the superficial subcutaneous layer 3:33 are called 3:33 subcutaneous or perianal abscess, and these are the most common. 3:39 Eorectal abscess are large and go from the superficial to the deep. 3:45 Superolevato abscess, as the names suggest, are abscess that occur above the 3:49 levato anti-muscle. 3:54 The formation of anorectal abscess can cause some signs and symptoms, including 4:00 severe 4:00 pain, especially when sitting. 4:03 The pain doesn't necessarily have to go with bowel movements. 4:08 There can be pain just whenever. 4:12 And there can also be fever, because as we know, an abscess is infection. 4:19 Another technical feature is malase and perulent discharge. 4:23 On physical examination, patients should be in a perrectal exam position, which 4:29 is lying 4:30 on the side, knees up to chest. 4:33 This will relieve the anal area. 4:37 And what is seen is potentially a fluctulence or patch of erythematous, endure 4:43 ated skin 4:44 within the buttock area. 4:45 And here, as shown, the abscess is on the left. 4:49 A digital rectal examination may also be performed, and this is to examine for 4:53 any deeper 4:54 abscess, and a digital rectal examination is done if there is suspicion of this 5:01 following 5:02 a general observation. 5:09 Diagnosis of abscess is generally straightforward. 5:11 Its history digs the examination, including anorectal pain, fever, and a 5:16 palpable anorectal 5:17 mass. 5:26 The pathophysiology of anal abscess. 5:29 Anal abscess usually originates from an infected anal crypt gland. 5:35 So here we have the crypts, and here we have the actual gland it connects to. 5:40 The anal crypt glands are situated roughly along the pectinate line. 5:45 The crypts themselves are tiny mucus glands of lubrication essentially. 5:50 So just before bowel movement, the sphinctum muscles contract and squeeze out a 5:54 little drop 5:55 of lubricating mucus from each of these crypts. 5:59 About 90% of all infections around the anorectum area originates from these 6:05 crypts. 6:05 And from these crypts, the bacteria can spread through the anal duct and then 6:11 infect the 6:12 glands. 6:13 And from here, the infection can spread really anywhere where there is least 6:19 resistance. 6:19 It can spread submucosally, subcutaneously, and transfinterically, or other 6:26 areas around 6:27 the tissue. 6:30 The general rule is that the abscess will collect in whichever anatomical site 6:37 the glands 6:38 terminate, or whichever path of least resistance is. 6:43 The differential diagnosis for anal rectal abscess include pilonidal cysts, hy 6:52 drinitis 6:53 supertiva, ortholenduct abscess in females, anal fissure, external hemorrhoids, 7:04 and fistula 7:05 in anal. 7:08 The management of anal abscess is basically drainage under local anaesthetic. 7:13 Antibiotics are used for groups at risk. 7:17 Further, fistulas can be identified using an anoscope by injecting fluid 7:23 through a visible 7:25 external opening and seeing where the fluid comes out from within the anal 7:30 canal. 7:31 If a fistula is identified, managing the fistula obviously comes with the whole 7:36 drainage 7:36 process. 7:40 Complication of anal rectal abscess includes spreading to other tissues, as 7:45 well as the 7:46 development of a fistula. 7:50 In this case, a intersfinteric abscess can cause an intersfinteric fistula. 7:56 Approximately 50% of patients with anal rectal abscess will develop a fistula, 8:02 and so assessing 8:03 or looking for a fistula and managing it together is very important.