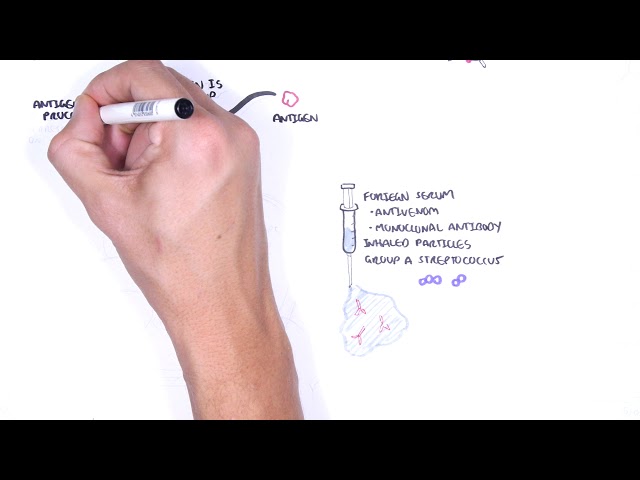
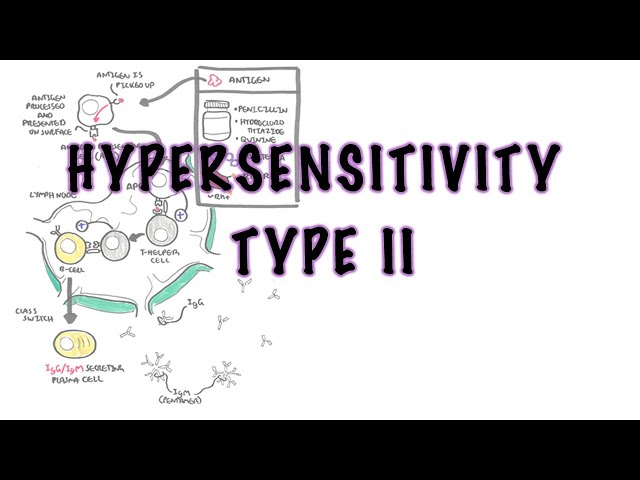
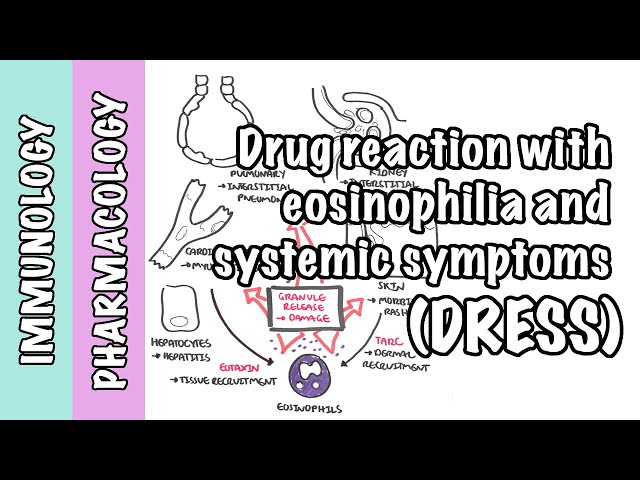
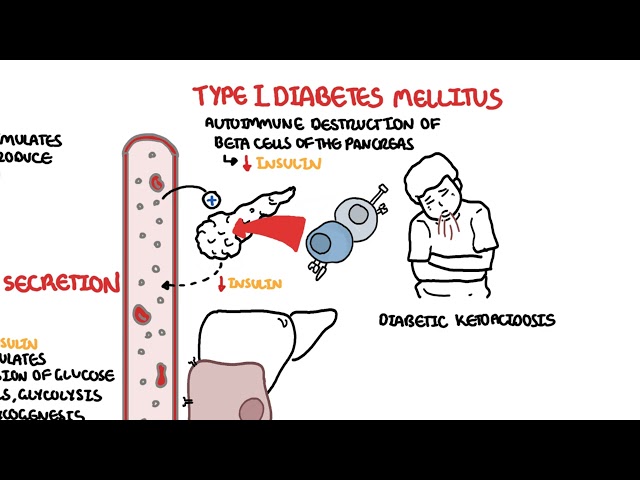
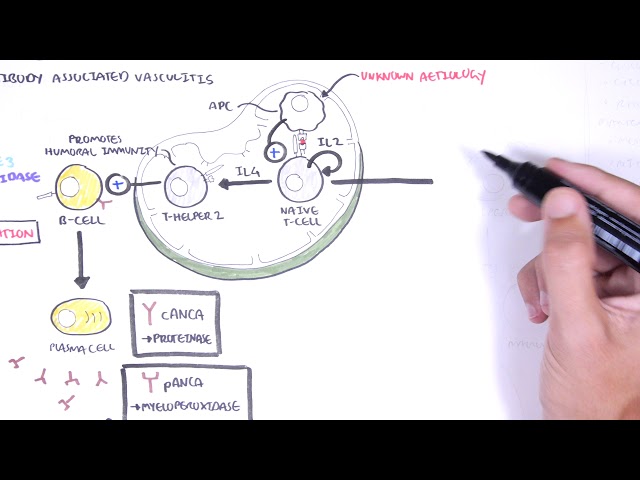
0:00 In this video, we're going to talk about hypersensitivity type 1. 0:15 Hypersensitivity reactions are exaggerated or inappropriate immune response to 0:20 benign 0:21 antigen. 0:22 It is the immune response and not the antigen that is actually harmful. 0:29 An external antigen such as a drug, pollen, or food can elicit an inappropriate 0:35 immune 0:35 response. 0:36 However, an inappropriate immune response to an internal antigen, such as your 0:42 own skin 0:43 or a neuron, would be called an autoimmune reaction. 0:48 Hypersensitivity reactions can be the mechanism of diseases in some autoimmune 0:55 reactions. 0:57 Hypersensitivity reactions are antigen-specific. 1:00 It's antigen-specific because the immune system is educated and primed towards 1:06 the antigen 1:07 after the first exposure. 1:10 In this quick example, first exposure or first contact to an external antigen, 1:15 such 1:15 as a drug, pollen, or food, causes the immune system to sensitize itself 1:22 towards the particular 1:23 antigen. 1:24 In other words, it primes the immune system against that antigen, so when the 1:30 next time 1:31 the antigen comes along, the primed immune system, including the T cells, 1:38 antibodies, 1:38 and neutrophils, they can mount an exaggerated and inappropriate immune 1:45 response, aka a hypersensitivity 1:47 reaction. 1:48 But the immune system can cause hypersensitivity reactions in different ways. 1:55 And that is why hypersensitivity reactions can be subdivided into four main 2:00 types. 2:01 Type 1, Type 2, and 3 hypersensitivity reactions are antibody-mediated, whereas 2:08 Type 4 is a 2:08 cell-mediated hypersensitivity reaction. 2:14 Hypersensitivity Type 1 is an antibody-mediated reaction. 2:18 It is also called immediate hypersensitivity reaction because it is fast. 2:23 An allergic reaction is a Type 1 hypersensitivity reaction, and really involves 2:28 recognition 2:29 of an antigen by primed IgE immunoglobulins on mast cells. 2:37 A scenario of an allergic reaction, which is a Type 1 hypersensitivity reaction 2:42 , involves 2:43 a first contact or first exposure to a particular benign antigen, such as a 2:51 pollen, a particular 2:53 food, or a particular drug. 2:55 Because this is how allergic reactions occur, let us call the antigen an aller 3:02 gen. 3:02 The allergen can be picked up by specialized antigen-presenting cells, which 3:07 process and 3:08 present part of the allergen molecule on the cell surface. 3:15 From here, the antigen-presenting cell will carry the allergen to nearby lymph 3:20 oid tissues 3:21 such as a lymph node, where the process of sensitization begins, and again, 3:27 sensitization 3:28 occurs from the initial exposure, first contact, to a particular antigen. 3:34 So the antigen-presenting cell presents the allergen to the T helper cells, 3:39 which will 3:40 then inform the B cells of this new allergen and will activate the B cells to 3:45 become plasma 3:47 cells via interleukin 21. 3:51 Interleukin 4 stimulates the B cells to class switch from an IgE, for example, 3:56 to an IgE 3:57 immunoglobulin. 4:00 The plasma cells are now IgE secreting plasma cells, which are primed 4:05 specifically towards 4:07 the particular allergen. 4:09 IgE is one of five immunoglobulin classes, and it has a major role in type 1 4:16 hypersensitivity 4:17 reaction. 4:18 IgE is made up of heavy chains and light chains, and on the top is the binding 4:23 site for that 4:23 specific antigen. 4:29 The other major player in the sensitization of the body, of the immune cells, 4:34 towards 4:35 the particular allergen are the mass cells, which are granular sites containing 4:39 mediators 4:40 called histamine. 4:43 On the surface of the mass cells are FC receptors, which are receptors for the 4:47 heavy chain of 4:48 IgE. 4:50 The heavy chain of IgE will bind on the FC receptor. 4:55 This does not activate the mass cells, rather the IgE sits there, and just ch 5:03 ills. 5:04 The IgE also binds firmly by its heavy chain, portion to receptors on the 5:11 surface of basophils. 5:14 Now, this completes the priming of the immune system towards that specific all 5:19 ergen. 5:20 The body is now ready and sensitized towards the particular allergen. 5:29 So now, on subsequent exposures to the allergen, what happens is that the bound 5:37 IgE on mass 5:38 cells will recognize the allergen, the allergen cross-links IgE on mass cell 5:45 surface, activating 5:46 these cells to degranulate and release their granules of histamine within 5:54 minutes. 5:56 Release of these fast mediators causes a number of things, including increasing 6:02 vascular permeability 6:03 and vasodilation, both of which causes edema and erythema to local tissues. 6:11 Release vascular permeability allows extravasation of neutrophils and other 6:16 acute inflammatory 6:17 cells and molecules, and this occurs very quickly. 6:22 The late phase of IgE mediated inflammation occurs within hours after exposure 6:28 to the allergen. 6:29 Here, other mediators are synthesized after the cells degranulate. 6:36 These mediators include leukotrines, prostaglandins from the arachidonic acid 6:42 pathway, as well 6:43 as isinophyll chemotactic factor anaphylaxis. 6:48 Leukotrines causes increased vascular permeability and bronchoconstriction. 6:53 Prostaglandins causes bronchoconstriction. 6:57 Isinophyll chemotactic factor of anaphylaxis attracts isinophylls to tissues 7:03 immediately. 7:04 All these mediators causes the variety of signs and symptoms we see in a type 1 7:10 hypersensitivity 7:11 reaction, which is an allergic reaction. 7:14 And this includes urticaria, eczema, angioedema, hay fever, and asthma, like 7:23 symptoms. 7:25 These reactions can be local or systemic. 7:29 A life-threatening cause of a systemic reaction to an allergen would be anaphyl 7:35 axis. 7:36 Anaphylaxis is the most severe form of type 1 hypersensitivity. 7:40 Here, people develop feeling of impending doom, hypotension, edema of the lips, 7:48 neck, 7:48 severe bronchoconstriction. 7:50 They can't breathe, as well as tachycardia, fast heart rate. 7:54 The person will develop anaphylactic shock. 7:57 Adrenaline needs to be administered quickly. 8:02 Another concept to understand is atopy. 8:04 Now atopy are immediate hypersensitivity reactions with both an environmental 8:09 trigger, as well 8:11 as a strong family predisposition. 8:14 Hay fever, asthma, and eczema tend to run in families. 8:19 And there are several processes which seem likely to play a role in atopy. 8:23 For example, dysfunction of the barrier leading to enhance antigen exposure to 8:30 the body. 8:31 Two, there can be increased uptake and presentation of external antigen, which 8:41 would sensitize 8:42 the immune response or immune system. 8:45 Three, there could be dysregulation of the T cells. 8:48 For example, people can have increased production of interleukin-4, which is a 8:53 cytokine responsible 8:54 for class switching to immunoglobulin EIGE. 8:58 And four, there can be hyper-responsiveness of target tissue to mediators and 9:04 cytokines. 9:05 And atopy is generally associated with elevated IgE, and large number of T 9:11 helper 2 cells. 9:13 So I hope you enjoyed that video on hypersensitivity type 1 reaction, which is 9:20 immediate reaction, 9:21 an allergic reaction. 9:23 Thank you for watching.