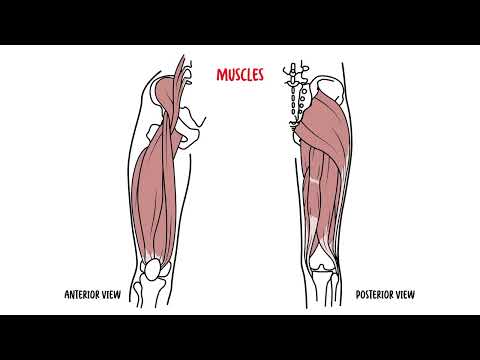
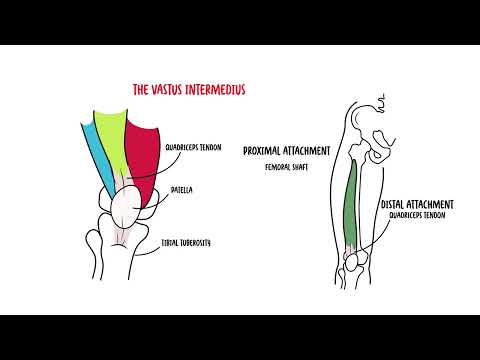
0:00 Hello, in this video, we're going to talk about the clinical anatomy of the 0:08 knee joint. 0:10 We'll begin by looking at an anterior view of the right knee. 0:15 The knee joint is made up of three bones, the femur, the patella, and the tibia 0:21 . 0:21 Here is the femur. 0:23 Because this is the right knee, and we are looking straight at it, it has a 0:28 medial 0:29 condal here, and a lateral condal here. 0:33 The patella articulates with the femur. 0:35 The patella is the biggest sesmoid bone in the body. 0:40 Here is a small bone, the fibula, which does not make up the knee joint. 0:44 Rather, it articulates with the tibia, the shin bone, which does make up the 0:49 knee joint. 0:50 The tibia has a tibial tuberosity here, which can get inflamed. 0:54 When it gets inflamed, it is known as "Oshkudshlata" syndrome. 1:01 Let's look at the same view of the right knee, so anterior view, but let's 1:05 introduce some 1:06 more structures. 1:09 The knee joint is special, because between the joints are fibrocartlaginous 1:14 structures 1:14 called menisca. 1:17 There is a medial and lateral meniscus. 1:22 These menisca are basically shock absorbers and help stabilize joint. 1:29 It also has a role in distribution of the synovial fluid. 1:34 The knee joint is further stabilized by many ligaments, the lateral collateral 1:38 ligament 1:39 here, and the medial collateral ligament here. 1:44 Here is the quadriceps tendon, which essentially attaches and over lies the p 1:50 atella bone, and 1:51 then forms the patella ligament. 1:53 The patella bone has a patella ligament, which runs and attaches to the tibial 1:58 tuberosity, 1:59 which as we discussed earlier, can get inflamed, and can undergo microevulsions 2:04 , which is characteristic 2:06 of "Oshkudshlata" syndrome. 2:09 The patella ligament is actually the continuation of quadriceps tendons, formed 2:15 by the rectus 2:16 femoris muscle, and the vastus muscles of the thigh. 2:22 Let us now look at the side view of the knee joint, and introduce the bursa. 2:28 The bursa are fluid-filled sacs that help reduce friction. 2:33 So here is the femur, tibia, and the patella. 2:37 The meniscus is the fibrocartlaginous structure that sits between the joints. 2:42 Here again is your quadriceps tendon, which comes down over and encapsulates 2:47 the patella 2:48 in front, forming the patella ligament. 2:52 Sometimes the patella ligament is also known as the patella tendon, and 2:57 essentially it 2:58 joins onto the tibial tuberosity. 3:02 The knee has a many bursa. 3:05 Here are some common ones, the supra-patella bursa, found above supra of the p 3:12 atella. 3:13 The pre-patella bursa, found on top of the patella bone, below the tendons and 3:19 skin. 3:20 And then you have your infra-patella bursa, which is below the patella. 3:25 And there are actually two, one deep and one superficial infra-patella bursa. 3:31 Clinically, the bursa can get inflamed, because of irritation between the skin 3:36 and bone, from 3:37 overuse and friction. 3:40 The pre-patella bursa can get inflamed, this is known as housemaid's knees. 3:45 This is because supposedly housemaids are on their knees and scrub the floor. 3:50 This will cause friction between the skin and the patella, leading to 3:53 inflammation of 3:54 the bursa between the two. 3:57 For a story, the infra-patella bursa can also get inflamed. 4:02 This one is known as a clergyman, bursitis, because of the same story, and 4:07 friction between 4:08 the skin and the tibia irritates the bursa, which lies between the two. 4:15 Let us now take our right knee joint again and look at it from an anterior view 4:21 , but 4:21 this time flexed, so bent. 4:25 In this position, we can introduce some other structures. 4:28 Again, here is the patella on top, because we are flexing the knee, and I'm not 4:34 drawing 4:34 the patella ligament here. 4:37 Here in blue is the medial and lateral meniscae. 4:42 Anteriorly is the transverse ligament, joining the anterior parts of the 4:47 lateral and medial 4:48 meniscus. 4:51 The relevance of this is that it supposedly prevents the meniscus from moving 4:55 forward. 4:59 Inside the knee joint, essentially we have two important ligaments, the 5:03 anterior cruciate 5:05 ligament, ACL, and the posterior cruciate ligament, PCL. 5:10 Remember this, they are named as to where they attach onto the tibia bone. 5:17 So the ACL ligament is a ligament which runs from the back of the femur and 5:23 attaches to 5:24 the front of the tibia, front as an anterior, hence anterior cruciate ligament. 5:30 The ACL prevents the tibia from sliding out in front of the femur. 5:36 The PCL runs, essentially, to the back of the tibia, from the femur, so the 5:42 posterior 5:43 of the tibia, hence posterior cruciate ligament, and the posterior cruciate lig 5:48 ament prevents 5:49 the knee from hyper-extending, so prevents the tibia from going behind the fem 5:59 ur. 5:59 Let's look at this from a different view, the right knee from the posterior 6:04 view, so 6:05 from the back. 6:06 Here again is the tibia, fibula, and intercondola knots, or the femoral notch 6:12 here. 6:13 Again, here in blue is your lateral and medial meniscus. 6:19 Coming off the posterior part of the lateral meniscus is the posterior menisc 6:25 ophamoral ligament, 6:27 a ligament which is known to have a secondary effect of a posterior cruciate 6:32 ligament. 6:33 And again, it comes off the posterior part of the lateral meniscus. 6:38 Anyway, and here is the PCL, the posterior cruciate ligament, which comes and 6:43 travels 6:43 from the medial femur to the posterior lateral part of the tibia. 6:52 The anterior cruciate ligament, on the other hand, comes from the lateral part 6:56 of the femur, 6:58 and travels and to row medially to the tibia. 7:03 Not only should you remember that ACL and PCL are named based on where they 7:08 attach to 7:09 on the tibial bone, but you should remember their course. 7:13 So what direction they travel in. 7:16 A good way to remember this is with the acronym LAMP, L-A-M-P. 7:22 L as in lateral, the A as in ACL moves medially. 7:33 LAMP as in medial, the P as in PCL moves laterally. 7:41 So LAMP might need some time to sink that one in. 7:47 So again, I'm going to draw another view of the anterior knee and introduce 7:52 some more 7:52 structures. 7:53 So here is the femur, tibia, and fibula again. 7:58 The medial condyle and lateral condyle here of the femur. 8:09 Here are your medial and lateral collateral ligaments. 8:13 An important area of the knee to remember, which is located at the anterior 8:19 medial part 8:19 of the tibia is the pest and serene, which consists of three muscle tendons, 8:27 semi-tendenosis, 8:28 gracilis and sartorius. 8:31 Behind these tendons sits the pest and serene bursa. 8:35 Clinically and quite common is the pest and serene tendinopathy or bursitis, 8:40 where there 8:41 is irritation of the pest and serene tendons and/or the bursa. 8:47 medial knee pain felt by climbing stairs and contracting hamstrings against 8:52 resistance 8:53 is a clinical feature. 8:55 The reason is because these muscles, these muscle tendons which attach to the 9:00 pest and 9:00 serene, works as hamstring muscles. 9:04 Finally, another important structure is the iliotibial band, which runs later 9:11 ally over 9:12 the lateral condyle and attaches to the anterior lateral part of the tibia. 9:20 The iliotibial band or ITB can get irritated at this point here, where it runs 9:25 over the 9:26 lateral condyle of the femur. 9:28 This can be a site of friction causing what is known as iliotibial band 9:33 syndrome or ITBS. 9:36 ITBS is a common overuse injury seen in cyclists and runners. 9:43 Here is a side view we are looking at the right leg laterally. 9:48 Here is the hip bone, gluteus maximus, quadriceps muscle and the biceps femoris 9:54 at the back. 9:55 Here is the tensor fascia lata. 9:58 One third of the tensor fascia lata and two thirds of the gluteus maximus. 10:04 The iliotibial joins and forms the iliotibial band which again attaches to the 10:10 anterior 10:11 lateral part of the tibia, but keep in mind that the site of friction of the 10:16 iliotibial 10:17 band is the lateral condyle of the femur. 10:22 The iliotibial band normally attaches to the tibia and helps stabilize and move 10:28 the knee 10:28 joint. 10:29 ITBS causes a sharp pain at the lateral condyle when a person squats at 45 10:35 degrees. 10:37 So bending, flexing, leads to the sharp pain. 10:41 This pain can be elicited and is tender at this angle too when pressed upon. 10:48 Now let us look at the posterior view of the right knee focusing on what is 10:53 known as a 10:53 popliteal fossa. The knee joint is surrounded by many muscles that help 11:00 stabilize the knee. 11:02 The lateral head of the gastrocnemus is here. 11:05 The medial head of the gastrocnemus is here, plantarus, biceps femoris and semi 11:10 -membranosis 11:11 just to name a few. 11:14 And running just next to the semi-membranosis is a semi-tendenosis which 11:21 attaches to at 11:22 the anterior medial part of the tibia, remember, and forms a pescensurine. 11:28 The popliteal fossa is essentially iphossa which contains things. 11:33 And the popliteal fossa is formed by the biceps femoris, superior latrally. 11:40 Superior medially, the semi-membranosis, inferior medially, the medial head of 11:46 the gastroc. 11:48 And inferior latrally is the plantarus and lateral head of the gastrocnemus. 11:55 So what is inside the popliteal fossa you ask? 11:59 Again here is the iliotibular band and the biceps femoris. 12:04 Now the tibion nerve runs here and branches to the common perineal nerve or the 12:10 fibular 12:10 nerve which then wraps around the latrally around the head of the fibular bone. 12:20 In the popliteal fossa, moving medially, we have the popliteal vein and then we 12:25 have 12:25 the popliteal artery which are continuations of the femoral vein and femoral 12:33 artery essentially. 12:35 More significance, while the popliteal fossa can swell up due to many reasons. 12:41 The most common being a bake assist which is essentially synovial fluid out p 12:47 ouching. 12:47 This resolves by itself with time and does not usually require surgery. 12:53 The other cause is a popliteal aneurysm which does need surgery. 12:58 When a person presents with a popliteal aneurysm, it is paramount to check for 13:03 aortic aneurysm 13:05 as in 50% of cases the person will have an abdominal aortic aneurysm. 13:11 Finally, let's continue talking about the common perineal nerve or also known 13:17 as the 13:17 fibular nerve which again is a branch of the tibial nerve at the popliteal foss 13:24 a. 13:24 As a common perineal nerve, the fibular nerve wraps around the head of the fib 13:30 ular latrally 13:30 it branches to the deep and superficial perineal nerves. 13:35 The deep perineal nerve supplies the anterior muscles of the leg and so is 13:41 responsible for 13:42 dorsiflexion and sensation in this area. 13:46 The superficial on the other hand supplies the lateral part of the leg so it is 13:50 responsible 13:51 for foot eversion and sensation around this area. 13:55 Clinical significance of foot drop can occur if there is damage or compression 14:00 to the common 14:00 perineal nerve also known as the fibular nerve. 14:06 So let's show an example. 14:08 Here we are looking at the left and right legs and feet from the top. 14:14 The left foot is normal and you can do dorsiflexion and foot eversion. 14:20 However, let's just say there is a problem or a damage such as a fracture to 14:27 the head 14:28 of the fibular you can damage the common perineal nerve. 14:32 And here obviously we are looking at the right lower limb. 14:38 So therefore the right leg the person who has damage to the common perineal 14:43 nerve on 14:44 the right side is unable to dorsiflex their right foot and also cannot do foot 14:51 eversion 14:52 as well they will lose sensation of the areas involved. 14:57 So I hope you enjoyed this video on the overview of Clinical Anatomy of the 15:01 knee. 15:01 Thank you for watching.