Dysphagia


Dysphagia, from the Greek dys (difficulty, disordered) and phagia (to eat), refers to the sensation that food is hindered in its passage from the mouth to the stomach. Dysphagia always indicates malfunction of some type in the oropharynx or esophagus, although associated psychiatric disorders can amplify this symptom. Dysphagia affects up to 15% of persons age 65 or older.
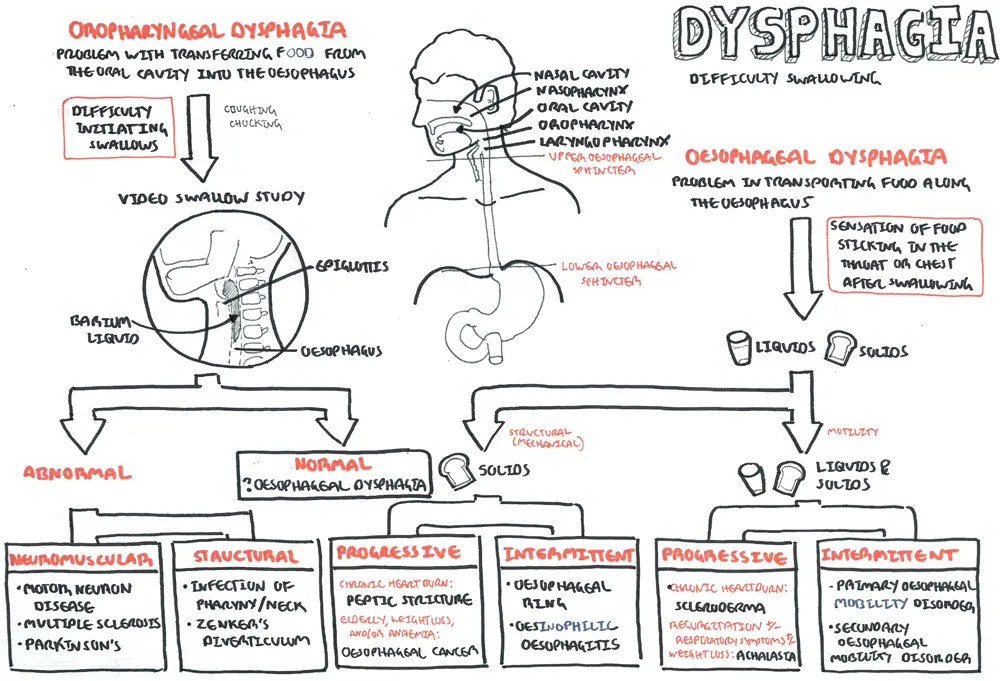
Dysphagia can be divided into oropharyngeal and esophageal dysphagia, although considerable overlap may occur in certain groups of patients.
| Think If a person can swallowing but has a sensation of food getting stuck and has difficulty moving the food down this is oesophageal dysphagia. Next, an attempt should be made to determine whether the patient has difficulty only with solid boluses or with both liquids and solids. |
| Oropharyngeal Dysphagia | Esophageal dysphagia |
| Coughing or choking with swallowing | Sensation of food sticking in the chest or throat |
| Difficulty initiating swallowing | Oral or pharyngeal regurgitation |
| Food sticking in the throat | Food sticking in the throat |
| Drooling/dribbling | Drooling |
| Unexplained weight loss | Unexplained weight loss |
| Changes in dietary habits | Change in dietary habits |
| Recurrent pneumonia | Recurrent pneumonia |
| Change in voice or speech | |
| Nasal Regurgitation or regress of fluid through the nose during swallowing | |
| Need to swallow repetitively to achieve satisfactory clearance |
| Remember recent onset of progressive dysphagia in the elderly is due to carcinoma of the oesophagus until proved otherwise. |
Oesophagus is a long tube that connect the pharynx to the stomach. It has three main contraction sites that help in moving the bolus (food) down to the stomach:
Cervical constriction: due to cricoid cartilage at the level of C5/6
Thoracic constriction: due to aortic arch at the level of T4/5
Abdominal constriction: at oesophageal hiatus at T10/11.
The oesophagus is divided into three parts:
Upper (Cervical): continuous with the oropharynx, commences at the lower border of cricoid cartilage (at level of C5/6) or cricopharyngeus muscle.
Middle (Thoracic): from thoracic aperture (T1) to the oesophageal hiatus (T10).
Lower (Abdominal): from oesophageal hiatus and is continuous with the cardia of thestomach at the gastro-oesophageal junction.
Blood supply Arterial supply
upper third: inferior thyroid artery
middle third: oesophageal branches of the thoracic aorta
lower third: oesophageal branches of the left gastric artery
Venous drainage upper third: inferior thyroid veins → brachiocephalic veins middle third: azygos vein → Superior Vena Cava lower third: left gastric vein → portal vein (portosystemic anastomosis)
| Remember Gastro-oesophageal junction is site of portosystemic anastomosis (between left gastric and (hemi)azygous veins)—may develop gastric or oesophageal varices if there is portal hypertension. |
The oesophagus is anatomically divided into three parts (cervical, thoracic, abdominal). However, it can also be divided into the upper two-thirds and lower one-third depending on histology. Upper two-thirds. Stratified squamous epithelial-lined (develops squamous carcinoma), striated skeletal muscle, lymphatic drainage to neck and mediastinal nodes, somatic innervation of sensation (accurate location of level of pathology). Lower third. Transition to columnar epithelium (develops adenocarcinoma), transition to smooth muscle, lymphatic drainage to gastric and para-aortic nodes, visceral innervation (poor localization of pathology). Upper oesophageal sphincter (UOS) = cricopharyngeus.Lower oesophageal sphincter (LOS) = functional zone of high pressure above the gastro-oesophageal junction.
Relaxants include alcohol. Anatomy of the oesophagus and surrounding structures
| Remember Swallowing requires intact and coordinated innervation from vagus (UOS, oesophagus, LOS) and intramural myenteric plexus. |
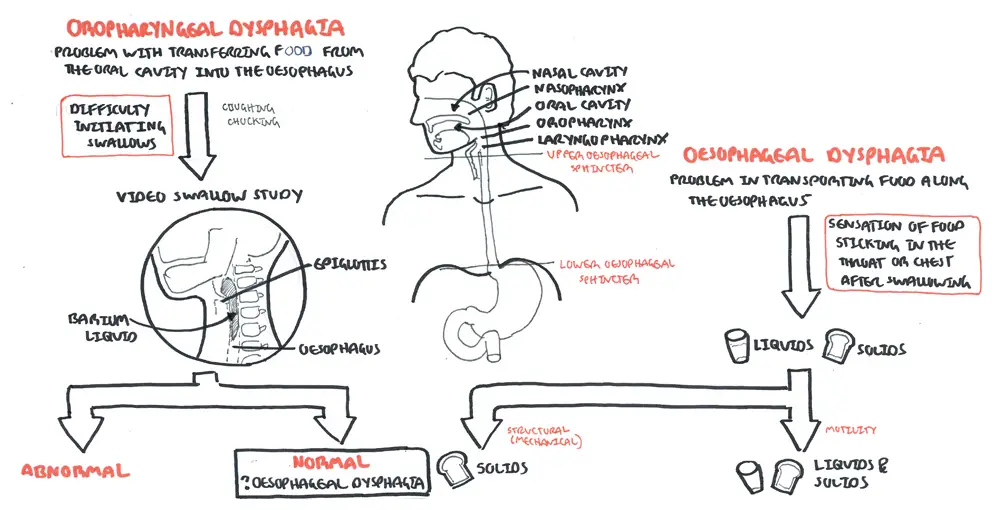
Oropharyngeal Dysphagia or “transfer dyphagia” is where the patient is often unable to initiate a swallow and repeatedly has to attempt to swallow. The patient is unable to transfer the food to the oesophagus.
| COMMON CAUSES OF OROPHARYNGEAL DYSPHAGIA | |
| Neuromuscular Causes* | Description |
| Motor Neuron Disease (ALS) | Amyotrophic lateral sclerosis (ALS) is a degenerative motor neuron disorder of adults. This condition commonly manifests itself in its early stages with dysarthria and dysphagia. These patients classically show progressive debilitation. |
| Gullian Barre Syndrome | |
| Multiple sclerosis | |
| Myasthenia gravis | Neuromuscular dysfunctions can also occur at the level of the neuromuscular junction; such is the case in myasthenia gravis. This is an autoimmune disorder in which antibodies that interact at the neuromuscular end plate are produced. This produces progressive weakness with repetitive muscle use. The most common presentations in the head and neck are ptosis, diplopia, dysarthria, and dysphagia. |
| Stroke | Central nervous system injury induced by hemorrhagic or ischemic stroke, both hemispheric and brainstem insults, can lead to dysphagia. At initial assessment, approximately 50% of stroke patients are at risk for aspiration. Over time, many of these patients improve such that by one week only one quarter of the patients remained at risk, and by 6 months less than 10% |
| Structural Causes | |
| Proximal oesophageal web | Oesophageal webs refer to an oesophageal constriction caused by a thin mucosal membrane projecting into the lumen |
| Oesophageal diverticula (Zenker’s) | A pouch, or pocket, of stretched tissue that develops anywhere along the esophagus, pushing outward through its muscular wall. They are rare, and can be congenital or acquired. Typically a single pouch forms, most often near the top of the esophagus; this is called Zenker’s diverticulum. |
Oesophageal Dysphagia
Problem in transporting food along the oesophagus. Sensation of food getting stuck in the throat, behind sternum or epigastrium after swallowing. It is then important to identify weather the problem is a motility (neuromusclar) or a mechanical (structural) problem. This is done with solid and water swallowing tests.
Motility and Mechanical Oesophagial dysphagia is further broker down to progressive and intermittent.
| COMMON CAUSES OF OESOPHAGEAL DYSPHAGIA | ||
| Motility (Neuromuscular) Disorders | Description | |
| Achalasia | Failure of relaxtion of lower esophagus during swallowing due to degeneration of myenteric plexus (nerves). It is characterized by non-peristaltic contractions in the smooth muscle segment of the esophagus and absent, incomplete, or abnormally timed lower esophageal sphincter relaxation in response to swallowing. | |
| Chagas’ disease | ||
| Scleroderma and other rheumatologic disorders | Diffuse esophageal spasm is characterized by replacement of normal peristaltic contraction by non- peristaltic contractions. Nonperistaltic contractions are not effective in causing normal esophageal transit. Characterised by severe chest pain and dysphagia | |
| Gastroesophageal reflux disease | ||
| Structural (Mechanical) Disorders | ||
| Carcinoma and benign tumors | ||
| Schatzki ring | Schatzki rings are fixed anatomic mucosal ring structures in the distal esophagus. They are distinct from lower esophageal muscular rings (A rings), which are transient, smooth, circumferential indentations in the esophagus. | |
| Eosinophilic esophagitis | Chronic inflammatory disorder of the esophagus and commonly classified as a Th2-type allergy. | |
| Goitre | ||
| Mediastinal tumours | ||
Two main investigations:
Other investigations:
Odynophagia: painful swallowing. Odynophagia may range from a dull retrosternal ache on swallowing to a stabbing pain with radiation to the back so severe the patient cannot eat or even swallow his or her own saliva.
| Causes of Odynophagia |
| Caustic Ingestion (acid/alkali) |
| Pill-Induced Injury |
| Infectious Esophagitis Viral – EBH, HIV, CMV Bacterial – TB Fungal – Candida albicans, Histoplasmosis Protozan – Bneumocystis, Cryptosporidum |
| Severe Reflux Esophagitis |
| Esophageal Carcinoma |

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion