75 year old presents to emergency with a 2 day history nausea, vomiting, abdominal pain and diarrhoea. He has not been tolerating oral fluids and is currently confused with a GCS of 14. He has a past medical history of heart failure, atrial fibrillation and chronic kidney injury. He is on digoxin, metoprolol and an ace inhibitor. Clinically he is dehydrated and in slow atrial fibrillation. Blood test shows he has acute kidney injury.
Overview
Overview Digoxin is from a family known as cardiac glycosides. Digoxin is derived from leaves of the purpule foxglove (digitalis pupurea) and inhibits the sodium potassium ATPase pump. Digoxin has positive ionotropic and negative chronotropic effect. Digoxin is used in two main conditions heart failure and tachyarrythmias such as atrial fibrillation. In heart failure the positive ionotrophic effect helps to increase cardiac output. In tachyarrythmias the negative chronotropic effects helps slow the heart rate. Digoxin toxicity has declined, possibly as a result of a decreasing use and a reduced recommended therapeutic range. Cardiac arrhythmias account for most deaths. Digoxin-specific antibody fragments are used when there is a risk of a life-threatening arrhythmia.
Pharmacology of Digoxin
Mechanism of action
- Na+/K+ ATPase inhibitor by competing with the K+ binding site
- Inhibition of pump causes increase intracellular Na+
- Increase in Na+ inhibits the Na+/Ca2+ pump causing an increase in intracellular Ca2+
- Increase in Ca2+ promote muscle contraction contraction
- Positive ionotrophy (stronger cardiac muscle contraction)
The inhibition of the Na+/K+ pump increases ionotrophy and prolonging action potential. By increasing ionotrophy and therefore increasing cardiac output the aortic arch and carotid sinus reflex arc is stimulated. This will increase parasympathetic tone and reduce SA and AV node firing slowing the heart rate
- Negative chronotrophy (reduces heart rate)
| Side note The Na+/K+ ATPase pump helps maintain membrane potential. It transports 3 sodium ions out of the cell for every 2 potassium ions that enter the cell. |
Metabolism
- Hepatic (but not dependent upon the cytochrome P-450 system)
Clearance
- The elimination of digoxin is mainly by renal clearance and is prolonged in patients with renal impairment.
ECG changes
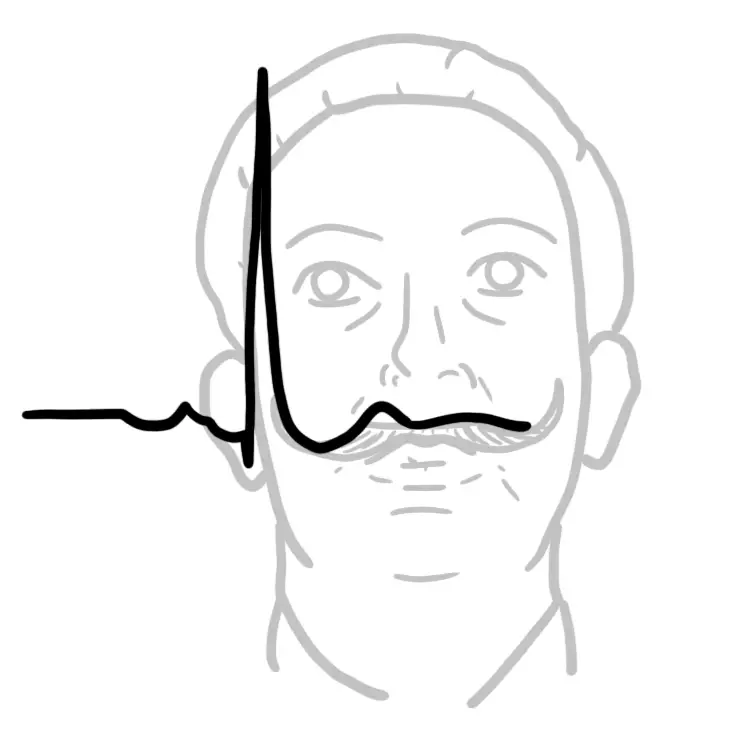
Therapeutic Digoxin ECG changes
- Scooped ST segment (Salvador Dali sign)
- Bibasic T wave (prominent U wave)
- Shortened QT
- AV block
| Remember Shortened QT is seen in hypercalcaemia as well |
Digoxin Toxicity ECG signs
- Premature ventricular contractions
- Sinus bradycardia
- AV block
- Slow Atrial fibrillation
- Ventricular tachycardia
Risk factors
Risk factors for digoxin toxicity
- Hypokalaemia
- Hypomagnesemia
- Hypercalcemia
- Acute kidney injury
- Many medications
- Amiodarone
- Indomethacin
- Spironolactone
| Think Hypokalaemia means that the K+ binding site in the Na+/K+ pump is more available to digoxin. This increases the effect of digoxin. |
Signs and symptoms
The therapeutic plasma concentration of digoxin is 0.5ng/mL – 1.0ng/mL. High levels of digoxin can lead to toxicity with arrhythmias being the most fatal.
| Visual | Neurological | Cardiovascular | Gastrointestinal |
| Double Vision | Fatigue | Bradycardia | Abdominal pain |
| Colour alterations | Confusion | Tachycardia | Anorexia |
| Haloes and scotomas | Weakness | Nausea and vomiting | |
| Headache | Diarrhoea |
| Remember Cardiac arrhythmias account for most deaths. |
Digoxin Toxicity arrhythmias include
- Premature ventricular contractions
- Sinus bradycardia
- AV block
- Slow Atrial fibrillation
- Ventricular tachycardia
The mechanism of tacharrythmias result from the electrophysiologic effects of digoxin: Increased intracellular Ca2+ levels predispose to Ca2+-induced delayed afterdepolarizations and hence increased automaticity. The mechanism of bradyarrythmias such as AV blocks is from excessive vagal tone.
Other complications
- Hyperkalaemia
Management
- Resuscitation
- Check potassium levels
- If hypokalaemia infusion with KCl
- If slow heart rate consider atropine
- In severe digoxin toxicity use digoxin immune Fab (Digibind)

Discussion