Overview
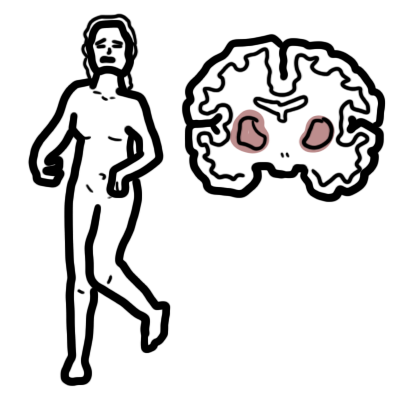
Cerebral palsy is a non-Progressive neurological disorder. Usually with significant motor component. Clinical presentation overtime changes due to increased developmental challenges.Cerebral palsy (CP) is the most common physical disability in childhood. Prevalence is about 1 – 3/ 1000 live births. Cerebral palsy can affect:
- Cerebral cortex – causing spasticity
- Basal ganglia – causing dyskinesia
- Cerebellum – causing akinesia
- Mixed
| Definition Cerebral Palsy: Group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain Dyskinesia: Abnormality or impairment of voluntary movement. Akinesia: Loss or impairment of the power of voluntary movement. Dystonia: A state of abnormal muscle tone resulting in muscular spasm and abnormal posture, typically due to neurological disease or a side effect of drug therapy. |
Anatomy and Physiology of the Motor Nervous system
| Watch Motor Pathway |
Classification
Cerebral palsy can be classified according to the type of motor problem:
- Spasitic (80%) – Cerebrum involvement
- Athetoid or dyskinetic (10-20%) – Basal ganglia involvement
- Ataxia (rare) – Cerebellar involvement
- Mixed
Cerebral palsy can be classified according to the distribution of motor disorder
- Hemiplegia
- Diplegia
- Quadriplegia
Aetiology
- Most causes are unknown
- Prenatal (ie. stroke, infection) most common
- Post delivery (i.e meningitis, kernicterus) 10-20%
- Perinatal asphyxia in minority (10%)
| Remember The majority of cerebral palsy is not related to birth asphyxia. |
Signs and symptoms
Common clinical presentation:
- Delayed motor milestones
- Asymmetric movement patterns
- Abnormal muscle tone
- Associated problems (poor feeding and irritability)
Signs and symptoms according to motor disorder
- Spastic Cerebral Palsy
- Increased deep tendon reflexes
- Tremors
- Muscular hypertonicity
- Weakness
- Characteristic scissors gait with toe-walking
- Athetoid or dyskinetic Cerebral Palsy
- Abnormally slow, writhing movements of the hands, feet, arms, or legs that are exacerbated during periods of stress and absent during sleep
- Ataxic Cerebral palsy
- Wide-based gait
- Intention tremors that complicate performance of daily activities requiring fine-motor function
In addition to motor manifestations, children with cerebral palsy frequently exhibit cognitive and sensory impairments, epilepsy, and nutritional deficiencies.
| Remember Intellectual impairment occurs in about two thirds of patients with cerebral palsy. About one half of pediatric patients have seizures. Growth problems are common, as well as neurologic abnormalities such as impaired vision or hearing and abnormal touch and pain perceptions. |
Differential Diagnosis
- Arginase deficiency
- Glutaric aciduria type 1
- VogtSpielmeyer disease
- Lesch-Nyhan syndrome
- Mitochondrial disorders
- Niemann-Pick disease type C
- Rett syndrome
Investigations and Diagnosis
Diagnosis of cerebral palsy is based on a clinical assessment, and not on laboratory testing or neuroimaging. Observation of slow motor development, abnormal muscle tone, and unusual posture are common initial clues to the diagnosis of cerebral palsy.
If differentials are suspected investigations may be ordered.
Complications and Prognosis
Associated impairments
- Intellectual and Learning disability
- Visual problems (45%)
- Hearing deficits (7%)
Health Problems
- Constipation
- Growth problems
- Gastro-oesophageal reflux
- Undecsenced testes
- Epilepsy
- Osteopaenia
- Mental illness
Motor disorder
- Urinary incontinence
- Spasticityand dystonia
- Tense muscles
Prognosis
The number of adults with cerebral palsy is increasing because of increased survival of low birth weight infants and increased longevity of the adult population. Adult mobility and ability to perform activities of daily living should be routinely monitored as the patient ages.
Mechanism of Disease
Management
Cerebral palsy is a chronic condition with no cure and as such the overall goal of treatment is to improve quality of life and participation in life situations. Management of cerebral palsy involves a disciplinary team:
- Physiotherapist
- Occupational therapists
- Speech pathologists
- Orthotists
- Social workers
- Nurses
- Psychologist
- Special education teacher
- Family physician
Management of complications
Associated impairments
- Intellectual and Learning disability – special education teacher
- Visual problems (45%) – visual assessment/glasses
- Hearing deficits (7%) – hearing assessment/screening
Health Problems
- Constipation – increase fluid intake, fiber, mobility and possibly introduce laxatives
- Growth problems – monitor feeding, might have to introduce feeding through nasogastric tube/gastrostomy tube
- Gastro-oesophageal reflux – antiemetic
- Undecsenced testes – Surgery
- Epilepsy – Anticonvulsants
- Osteopaenia – monitor vitamin D levels, introduce faily sun exposure
- Mental illness – psyhcologist
Motor disorder
- Urinary incontinence
- Tense muscles – Orthopaedic referral for hips, knees, ankles which are most commonly affected
- Botulinum toxins for localised spasticity or focal dystonia
- Anticonvulsants




Discussion