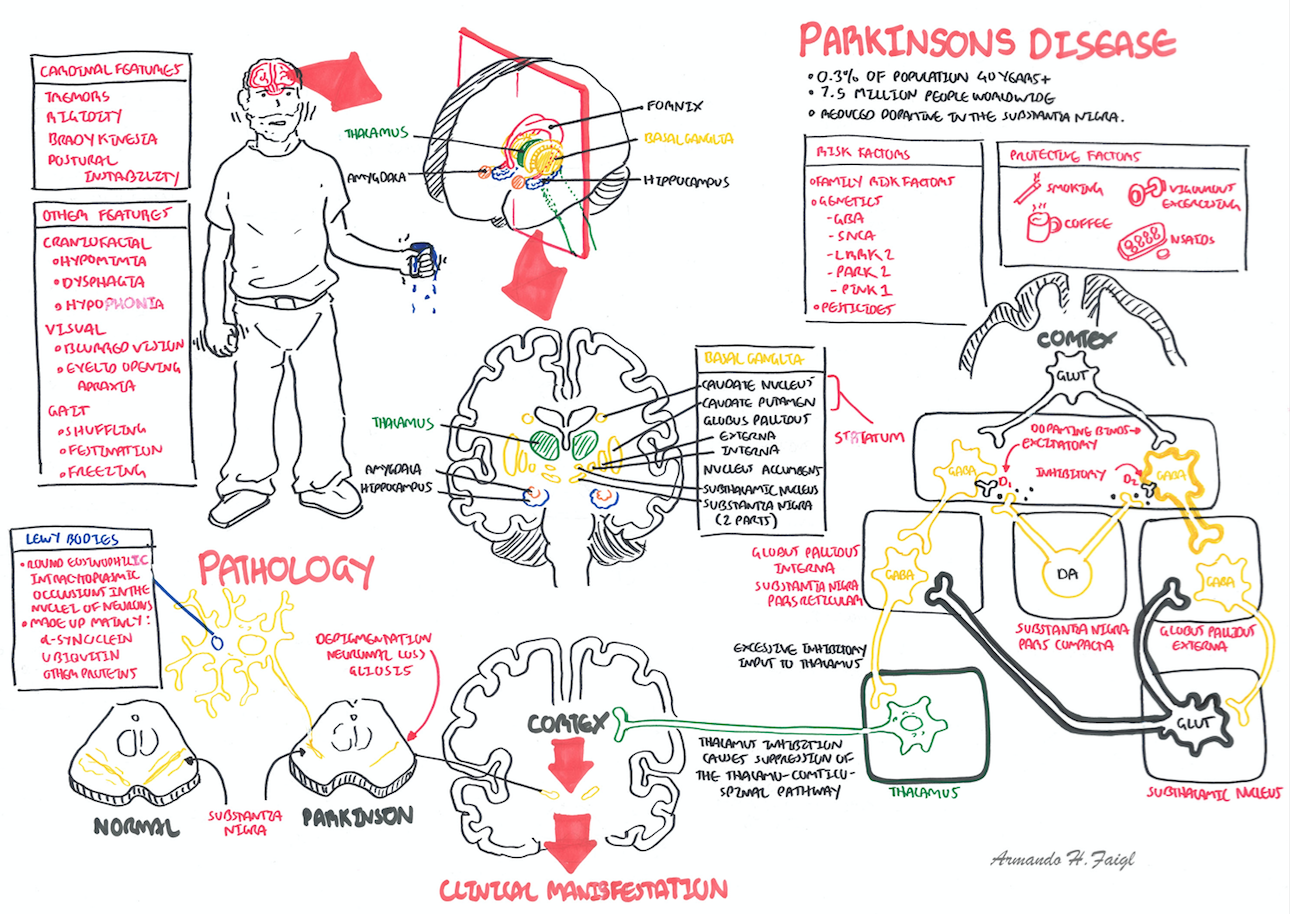
Overview Parkinson’s disease is a progressive neurodegenerative disorder characterised by tremor, rigidity, bradykinesia, and a wide spectrum of non-motor symptoms including sleep disorders, hyposmia, bladder and bowel dysfunction, fatigue, dementia, and other neuropsychiatric symptom. Although the disease has no cure, available treatments effectively control motor symptoms and improve quality of life. Parkinson disease affects approximately 1 percent of persons older than 60 years, and up to 4 percent of those older than 80 years.
| Remember Parkinson's disease should be suspected in someone with tremor, stiffness, slowness, balance problems, or gait disorders |
| Definition Parkinson's Disease: or Idiopathic Parkinson's disease is a progressive, degenerative brain disease that causes trembling, stiffness, slowness of movement and a loss of fine motor control. It is the most common type of parkinsonism. Unlike some other forms which have specific causes it is not known why idiopathic Parkinson's occurs. Parkinsonism: Umbrella term that describes many conditions which share some of the symptoms of Parkinson's. The main symptoms of Parkinson's – tremor, rigidity and slowness of movement – are also the main symptoms of a number of conditions that are grouped together under the term parkinsonism Akinetic Rigid Syndrome: Defined by paucity and slowness of movement accompanied by muscle stiffness and resistance to passive movement. The akinetic–rigid syndrome is typical of idiopathic Parkinson's disease, so is often described as the syndrome of parkinsonism. Parkinson's - Plus Syndrome: neurodegenerative conditions with Parkinson's characteristics but with additional features that distinguish them from idiopathic Parkinson's disease. Usually they are not responsive to dopamine. |
| ↑Risk | ↓Risk |
| Pesticides | Smoking |
| Rural residence | Caffiene |
| Farming | |
| MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) |
| Four Cardinal Signs of Parkinson's: Resting Tremor, Bradykinesia, Rigidity and postural Instability. |
Pre-motor features of PD
| Remember Rapid eye movement (REM) sleep behavior disorder a prodromal syndrome of alpha-synuclein neurodegeneration including parkinsnon's disease and some parkinson's plus syndrome. REM sleep behaviour disorder is characterized by dream-enactment behaviors that emerge during a loss of REM sleep atonia. |
4 cardinal motor symptoms (more info below)
Resting Tremor
Bradykinesia
| Glabellar reflex is a primitive reflex. It is elicited by repetitive tapping on the forehead. The tapping causes the person to blink but after a while blinking stops. In Parkinson's Disease blinking persists. |
Rigidity (Stiff joints)
Postural instability
Non-motor signs/Autonomic dysfunction
Tremor, often combined with slowness and stiffness in an arm, presents frequently in general practice. It may be caused by essential tremor, which affects 2-3% of the population. Differentiating essential tremor from Parkinson's disease can be difficult, even for experienced physicians.
Essential tremor (ET)
| CAUSES OF PARKINSONISM | |||
| Condition | History | Signs and symptoms | Radiological findings |
| Idiopathic Parkinson’s disease | Difficulty with tasks, rigidity, tremor | Resting tremor, rigidity, bradykinesia | No specific CT or MRI findings |
| Drug-induced parkinsonism | Previous use of a causative drug such as an antipsychotic, reserpine or metoclopramide | Tremor, rigidity, bradykinesia; often bilateral symptoms | None |
| Vascular parkinsonism | Stepwise progression; CVA or TIA, comorbid cardiovascular disease | Fixed deficits from previous events | Lesions in white matter +/- basal ganglia |
| Parkinson's Plus syndrome | |||
| Normal-pressure hydrocephalus | Ataxia, dementia, urinary incontinence | Ataxic gait, change in mental status | CT or MRI shows hydrocephalus |
| Dementia with Lewy bodies | Cognitive impairment, hallucinations, episodes of delirium, parkinsonism | Impaired attention and visuospatial abilities, increased falls, episodes of syncope | PET shows low glucose metabolism in cortex |
| Remember Drug-induced parkinsonism is symmetric, lacks nonmotor features, and is reversible after removal of the causative agent. Typical antipsychotics, also known as neuroleptics, are the most common causes of DIP |
Investigations
| Side note DaTscan is a dopamine transporter (DAT) single photon emission computerized tomography (SPECT) imaging technique. It provides a potential tool to evaluate patients with unclear PS symptoms. It can be used to differentiate between disorders of essential tremor or drug induced PS. |
Clinical Diagnosis
These features are unilateral at onset, but become bilateral as the condition progresses. Later, postural instability and falls, orthostatic hypotension, decreased olfaction, micrographia and dementia (Lewy bode dementia)
| Side note Imaging plays a limited role in diagnosis and should not be used routinely. |
Hallmarks of PD are the presence of Lewy bodies + neuronal cell death in the pars compacta of the substantia nigra.
PD does not develop until striatal dopamine (DA) levels drop to 20% and substantia nigra (SN) cell loss exceeds 50%.
| Watch Parkinson's Disease Pathophysiology |
Multidisciplinary team
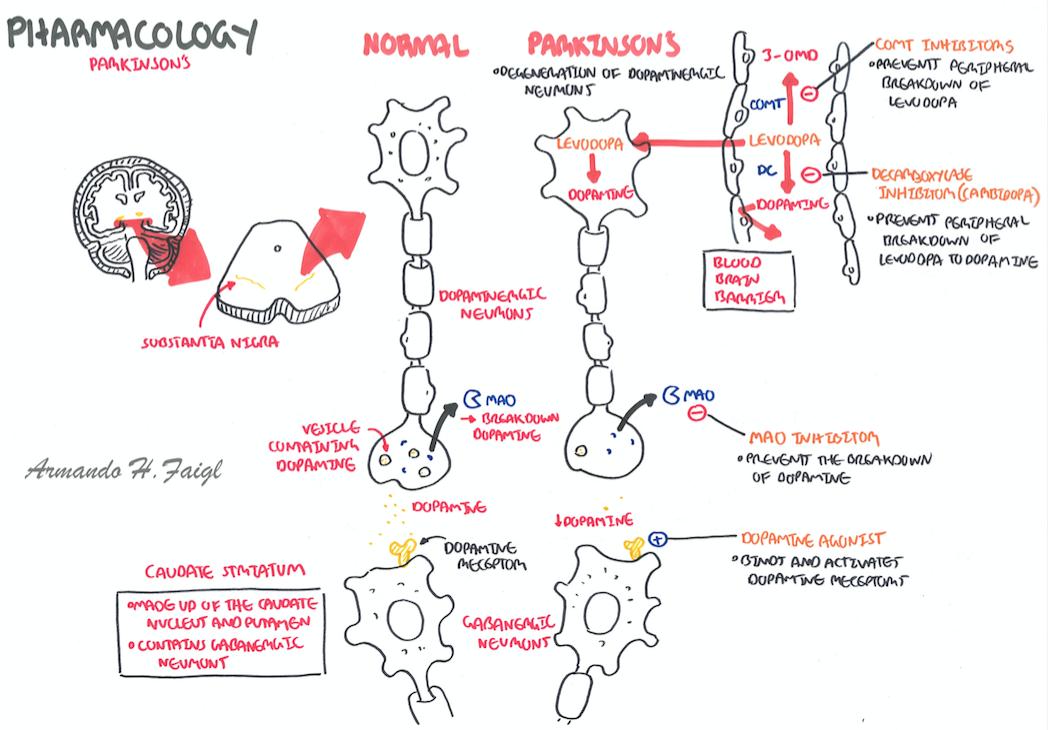
Pharmacological Treatment
| Remember Monitor for motor complications (dyskinesias, motor fluctuations) and impulsivity and adjust doses accordingly |
| Remember For Parkinson's disease who have new troublesome hallucinations or delusions, a precipitant such as an underlying delirium, infection or dementia should be ruled out. Then, if able, anti-Parkinsonian medications should be adjusted. If despite this the delusions continue, then options include treatment with quetiapine, clozapine, or pimavanserin. Other antipsychotics will worsen Parkinsonian symptoms. |
Other Pharmacological Treatment
| Side Note Motor complications develop in 50% of all PD patients after 6 years of levodopa therapy |
| Pharmacology Levodopa Side-effects: nausea, vomiting, anorexia. Long-term complications of Levodopa: Dyskinesias, Dystonia, Unpredictable on/off switching, Confusion, Visual hallucinations, Delusions, Illusions |
| Pharmacology Dopamine Agonists directly stimulate dopamine receptors Side effect: nausea, vomiting, postural hypotension, confusion, hallucinations and impulsivity, somnolence |
| Remember Do not stop treatment abruptly because this may cause neuroleptic malignant syndrome, which is then treated with dantrolene and bromocriptine (dopamine agonist) |
| Watch Pharmacology - anti parkinson drugs |
Surgical Treatment
Complications
| Neuroleptic malignant syndrome should be considered in patients taking antipsychotic medications (dopamine antagonist) or for those who stop taking dopamine replacement medications suddenly. Clinical manifestation include fever, rigidity, altered mental statu, autonomic dysfunction (hypersalvation, urinary incontinence), and elevated creatine phosphokinase concentration |
Prognosis
| Freezing occurs when patients are unable to move their feet when trying to walk. It affects half of all people who have Parkinson's disease |
Overview Essential tremor is an important differential from a pill rolling parkinson tremor. Postural or kinetic tremor in the frequency range of 4 to 12 Hz (usually at the lower end of the range in older patients) is generally the only manifestation in patients with essential tremor. Occasionally, when severe, rest tremor and mild abnormalities of tone and gait may also occur. A family history of this disease and temporary benefit after drinking alcohol are common, but not invariable.
Management
