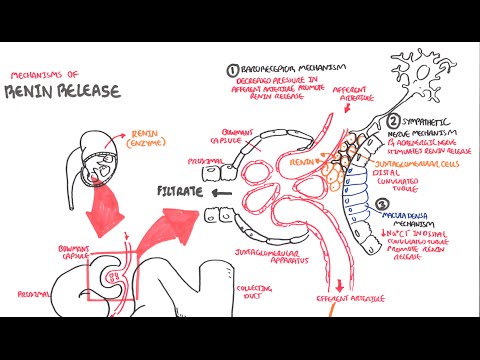
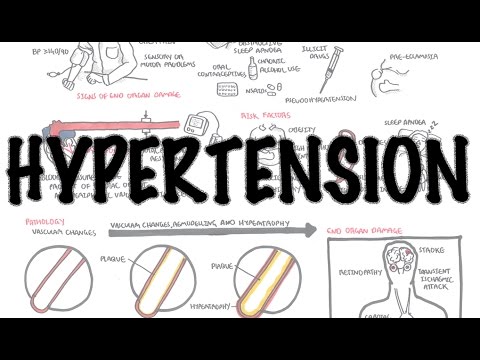
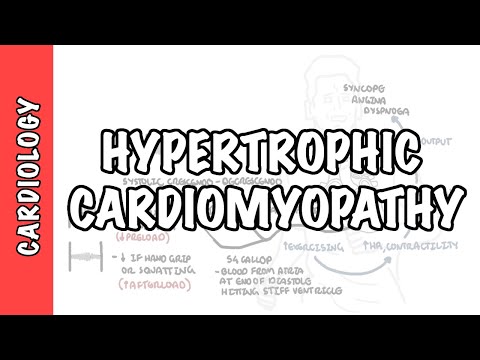
0:00 Hello in this video, we're going to talk about cardiorenal syndrome. 0:15 Acute or chronic dysfunction of the heart can lead to acute or chronic 0:19 dysfunction of 0:20 the kidneys and vice versa. 0:23 Acute or chronic dysfunction of the kidneys can lead to acute or chronic 0:26 dysfunction of 0:27 the heart. 0:28 A few associations have been made between the heart and the kidneys. 0:31 These are that mortality is increased in patients with heart failure who have a 0:36 reduced glomerular 0:37 filtration rate. 0:39 Patients with chronic kidney injury have an increased risk of both atheroscler 0:43 otic cardiovascular 0:44 disease and heart failure and cardiovascular disease is responsible for up to 0:48 50% of deaths 0:49 in patients with renal failure. 0:54 Acute or chronic systemic disorders can cause both cardiac and renal 0:58 dysfunction. 0:59 Basically, a diseased heart has numerous negative effects on kidney function, 1:05 but at the same 1:05 time renal insufficiently can significantly impair cardiac function. 1:12 Given the complex nature and association between the heart and the kidneys, a 1:15 group of cool 1:16 guys categorize the different interactions between the heart and kidneys into 1:21 five types. 1:22 So these are the five types of cardio renal syndrome. 1:25 Type one is when you have acute heart failure causing acute kidney injury. 1:30 Type two chronic heart failure causing chronic kidney injury. 1:36 Type three abrupt or worsening acute kidney injury can lead to sort of an acute 1:43 cardiac 1:43 dysfunction such as a heart failure. 1:48 Type four cardio renal syndrome is when you have chronic kidney disease 1:52 contributing 1:53 to cardiac dysfunction which can manifest as coronary artery disease, heart 1:57 failure or 1:58 arrhythmias. 1:59 Type five is when you have essentially a systemic disorder such as sepsis or 2:04 diabetes that can 2:06 cause both cardiac and renal dysfunction. 2:10 In this video, we'll focus on type one and type two cardio renal syndrome which 2:15 is where 2:15 the heart dysfunction causes renal dysfunction and then we can touch on type 2:20 four where 2:21 chronic kidney disease contributes to basically cardiovascular disease. 2:29 So heart failure is when there is not enough cardiac output to meet metabolic 2:34 demand. 2:34 Cardic output is calculated by heart rate times by stroke volume. 2:39 Card volume is affected or the factors of stroke volume include the preload, 2:45 contractility 2:46 and afterload. 2:51 In acute heart failure such as after a myocardial infarction, infection or 2:56 complications from 2:57 surgery, you have a sudden drop in cardiac output and you will get all these 3:03 symptoms 3:04 of heart failure. 3:10 With a drop in cardiac output, the sympathetic nervous system activates and 3:15 will increase 3:16 stroke volume and will increase heart rate to compensate as well as it will 3:24 stimulate 3:24 the release of renin from the kidneys. 3:27 The release of renin will activate the renin androgen syndrome system but this 3:31 takes a 3:32 while. 3:34 Further with reduced cardiac output and heart failure, there is reduced perf 3:38 usion to the 3:38 kidneys which will subsequently lead to acute kidney injury. 3:44 And this is already the beginning of the relationship, the cardio renal 3:48 syndrome. 3:49 With reduced perfusion, renin is released as well, activating the renin and 3:54 rogen and 3:55 aldosterone system or RAS for short. 4:00 RAS leads to an increase in sodium and water retention and it will also 4:05 increase ADH, antidiuretic 4:07 hormone, which will aim to increase the mean arterial pressure, the blood 4:11 pressure essentially. 4:14 However, while water and sodium increases the volume, it will also increase the 4:19 mean 4:19 arterial pressure which means that there will be an increase in afterload which 4:24 technically 4:24 reduces cardiac output. 4:28 RAS also causes vasoconstriction, further contributing to reduced renal perf 4:36 usion. 4:36 When you have right-sided heart failure, it means that you have an increase in 4:42 central 4:42 venous pressure because blood will sort of go backwards and when you have an 4:46 increase 4:47 in central venous pressure, you have an increase in renal vein pressure which 4:51 will contribute 4:52 to acute kidney injury. 4:56 Vasoconstriction from RAS also will increase mean arterial pressure. 5:02 During heart failure, the ventricles stretch and release brain naturally pept 5:06 ide and the 5:07 vessels as well as the heart release other vasodilatory mediators such as nit 5:12 ric oxide, 5:13 prostaglandins and bradykinin. 5:17 Now these mediators will mitigate the renin angiotensin-eldosterone system 5:24 technically, 5:24 however given the ongoing reduced cardiac output, which also is compounded by 5:29 the acute 5:30 kidney injury, these vasodilatory mediators don't really have much of an effect 5:35 and the 5:36 renin angiotensin-eldosterone system will predominate. 5:42 Acute heart failure as well as other heart failures have an inflammatory 5:44 component to it, 5:46 driven by the innate immune system contributing to acute kidney injury. 5:53 In acute heart failure, exogenous factors also causes acute kidney injury. 5:58 This can be from contrast from emergency angiograms as well as the use of neph 6:06 rotoxins. 6:07 As you can see, there are many mechanisms of acute kidney injury when acute 6:10 heart failure 6:11 occurs. 6:12 But the same principle or mechanisms happens with chronic heart failure, with 6:17 the activation 6:18 of the renin angiotensin-eldosterone system playing a big role. 6:25 Continuing on though, prolonged acute kidney injury can lead to chronic kidney 6:30 disease. 6:31 Now as we know, chronic kidney disease can occur from many other causes, 6:36 diabetes, hypertension 6:38 and glomerular nephritis. 6:41 Type three and type four cardio renal syndrome. 6:44 Look at how acute kidney injury and chronic kidney injury causes cardiac 6:52 dysfunction. 6:53 Let's focus on type four, which is how primary chronic kidney disease can lead 7:01 to essentially 7:03 cardiovascular dysfunction. 7:05 So chronic kidney disease is defined by low glomerular filtration rate. 7:11 Low glomerular filtration rate will activate the renin angiotensin-eldosterone 7:16 system. 7:16 The renin angiotensin-eldosterone system will do a few things. 7:19 Firstly, it will cause systemic vasoconstriction, which is hypertension. 7:27 Hypertension causes cardiac remodeling. 7:30 Cancer and sodium retention increases the menotria pressure, hypertension, and 7:35 also will 7:36 affect cardiac muscle cells leading to cardiac remodeling, as well as left vent 7:41 ricular hypertrophy. 7:44 Chronic kidney disease leads to reduced erythropoietin production, which will 7:50 lead to anemia. 7:52 And so you have an increased risk of ischemic events, technically in the heart. 7:58 Chronic kidney disease also means that you have less active vitamin D, leading 8:03 to elevated 8:04 parathyroid hormone levels. 8:06 When you have elevated parathyroid hormone levels, this causes an increase in 8:09 calcium 8:09 and phosphate, which can increase coronary and tissue calcification, leading to 8:14 an increased 8:15 risk of ischemic events. 8:18 In kidney disease, you have electrolyte imbalance. 8:22 And specifically, hyperkalemia can lead to arrhythmia within the heart. 8:29 In summary, these changes increase the risk of cardiovascular disease, chronic 8:33 heart failure, 8:34 coronary artery disease, and arrhythmias. 8:38 Management of cardiorenal syndrome is challenging, because treatment directed 8:43 towards improving 8:44 cardiac function can worsen kidney function. 8:48 Step one and type two cardiorenal syndrome is what we will mainly focus on. 8:55 So in this scenario, diuretics is obviously used if there is fluid overload. 9:02 And we know that it will cause renal impairment. 9:05 Asinhibitors or angiotensin-receptor blockers are used in heart failure. 9:11 And it may improve glomerular filtration rate temporarily, but does not improve 9:16 renal function 9:17 technically. 9:19 They are also nephrotoxic, and their mechanism is essentially that they cause 9:24 vasodilation 9:25 of the ephrin arterioles, essentially relieving pressure in the glomerulus. 9:36 In cardiorenal syndrome, the use of intravenous vasodalas may also help. 9:42 cardiorenotropic drugs are only used for cardiogenic shock in heart failure. 9:49 And then you have ultra filtration, and this is usually for patients with 9:53 decompensated 9:54 heart failure who are diuretic resistant and require fluid to be offloaded. 10:01 Thank you for watching. 10:02 I hope you enjoyed this video on cardiorenal syndrome, which is quite 10:05 complicated. 10:06 But as you, as we've learned, there's five types. 10:09 And type 1 and type 2 are probably the most worth knowing about, as well as 10:13 type 4 cardiorenal 10:15 syndrome. 10:16 Thank you for watching. 10:17 I hope you enjoyed this video.