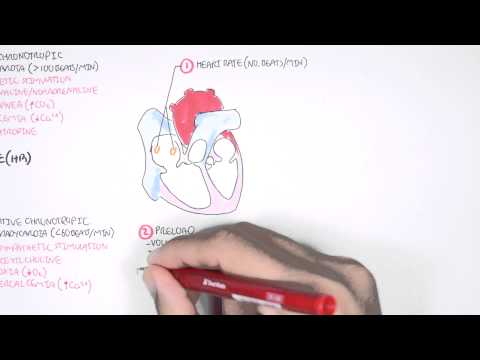
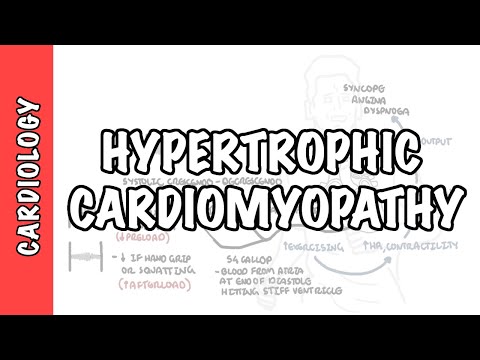
0:00 Heart failure is a disorder in which the heart cannot pump blood to the body at 0:09 a rate that 0:09 is needed. 0:10 It is a clinical syndrome caused by a variety of cardiac diseases and causes 0:14 characteristic 0:15 symptoms of dyspnea and fatigue. 0:18 Clinically, heart failure is divided into two broad categories, heart failure 0:22 with reduced 0:23 ejection fraction and heart failure with preserved ejection fraction. 0:28 In this video, we will focus on heart failure with preserved ejection fraction, 0:32 which accounts 0:32 for more than 50% of heart failure cases. 0:36 To better understand heart failure, we need to review the heart's function. 0:42 The heart has two phases during each heartbeat, filling, which is diastole, and 0:48 pumping, which 0:49 is systole. 0:51 Cystolic function of the heart and resulting cardiac output is governed by four 0:55 major determinants. 0:57 These are the contractility of the heart muscle, the preload of the ventricle, 1:03 and then the 1:03 afterload, which is the force the ventricles must overcome to pump blood out, 1:08 and finally 1:09 the heart rate. 1:11 The cardiac output equation can be simplified nicely into stroke volume, which 1:16 is the amount 1:16 of blood the ventricles pump out during each heartbeat, multiplied by heart 1:23 rate. 1:24 Safety, afterload, and preload all affect stroke volume. 1:32 Low cardiac output is the main feature in heart failure. 1:35 The heart fails to pump blood to the rest of the body. 1:39 Cardiac output may be inadequate as a result of any alterations in the determin 1:43 ants we 1:43 talked about. 1:48 Heart failure with preserved ejection fraction is a problem with diastolic 1:52 function, a problem 1:54 with heart filling typically. 1:58 The most common cause of heart failure with preserved ejection fraction is 2:02 hypertension 2:03 and less commonly aortic stenosis. 2:07 These changes cause an increase in afterload, which causes slow adaptations to 2:11 the ventricles. 2:13 An increase in afterload means stroke volume will decrease. 2:17 This means that the cardiac output will decrease. 2:22 A reduced cardiac output will be picked up by baroreceptors. 2:26 The baroreceptors will then trigger activation of the sympathetic nervous 2:31 system, which will 2:32 subsequently increase contractility of the cardiac muscles, increase the heart 2:39 rate as 2:39 well as venous tone. 2:45 These are all done to help increase cardiac output. 2:50 Long term, however, these changes causes ventricular remodeling and dysfunction 2:58 . 2:58 In addition to this, reduced cardiac output means that those reduced renal perf 3:03 usion. 3:04 As a result, the kidneys will activate what's called the renin angiotensin-eld 3:08 osterone system. 3:10 This is in the hopes to also increase cardiac output, however long term, again, 3:14 causes ventricular 3:16 remodeling. 3:17 The ventricular muscles of the heart specifically undergo what's called concent 3:22 ric remodeling 3:23 and hypertrophy, causing a smaller ventricular size. 3:28 This means less blood in the ventricles. 3:32 The hypertrophy muscle cells fibros due to inadequate blood supply, as a result 3:38 there 3:38 is stiffness of the ventricles and reduced compliance, so less blood filling 3:44 the ventricle 3:45 during diastole. 3:49 The reduced ventricular compliance, as a result of ventricular stiffness, 3:53 causes an increase 3:55 in ventricular pressure, which then will cause increase in arterial pressure, 4:02 and this can 4:03 lead to pulmonary congestion. 4:06 Majority of patients with heart failure with preserved ejection fraction 4:11 suffers from pulmonary 4:13 hypertension, and as a result, can develop right ventricular dysfunction, right 4:18 -sided 4:18 heart failure. 4:20 Of course, we cannot forget there's also left-sided dysfunction, as a result of 4:24 the ventricular 4:25 remodeling process as well. 4:29 Overall there is diastolic dysfunction, reduced volume of blood in the ventric 4:34 les, and therefore 4:35 overall reduced stroke volume and cardiac output. 4:39 However, the ejection fraction, which is the percentage of blood volume ejected 4:44 by the 4:45 heart during each cardiac cycle, is normal. 4:48 And this is because the heart is still able to pump the small volume of blood 4:51 during systole. 4:53 Hence why this heart failure is called heart failure with preserved ejection 5:03 fraction. 5:05 And so the pathological classification of heart failure is based on ejection 5:10 fraction. 5:11 Patients with chronic heart failure can either be heart failure with reduced 5:14 ejection fraction 5:15 or heart failure with preserved ejection fraction. 5:18 Heart failure with reduced ejection fraction is where there is impaired syst 5:22 olic function, 5:23 impaired emptying represented by an ejection fraction less than 40%. 5:30 Heart failure with preserved ejection fraction is an impairment in filling, but 5:36 you have preserved 5:37 ejection fraction of greater than 50%. 5:40 The distinction is important because the treatment of these two groups are 5:44 different. 5:45 Patients with ejection fraction of 41 to 49% are classified as preserved eject 5:50 ion fraction, 5:52 and their treatment is usually under this category as well. 5:56 Heart failure with preserved ejection fraction, previously known as diastolic 6:00 heart failure, 6:01 accounts for approximately 50% of all heart failure cases. 6:05 The most common cause is hypertension, less common aortic stenosis, and then 6:10 cardiomyopathy 6:11 such as hypertrophic obstructive cardiomyopathy, restrictive and infiltrative 6:18 cardiomyopathies. 6:20 Heart failure with preserved ejection fraction is also associated with other 6:24 conditions such 6:25 as obstructive sleep apnea, diabetes and obesity. 6:35 Clinical signs and symptoms of heart failure is easily classified into left- 6:39 sided heart 6:40 failure or right-sided heart failure. 6:44 Left-sided heart failure has symptoms of low cardiac output and elevated 6:48 pulmonary venous 6:49 pressures or pulmonary congestion. Low cardiac output state causes presyncopy, 6:56 fatigue and 6:57 lethargy, exertional dyspnea which will progress to orthopnea and parachysmal 7:02 noctinal dyspnea. 7:05 Pulmonary edema causes shortness of breath and chest discomfort, chronic non- 7:09 productive 7:09 cough, coarse crackles at the base and hypoxia. 7:16 Right-sided heart failure causes congestion of peripheral tissue and this 7:20 manifests as 7:21 a raised jugular venous pressure, liver congestion with a sustained pulsedile 7:27 liver, right ventricular 7:28 heave and lower limb pitting edema. 7:38 Investigations to order include a brain-naturtic peptide which is released by 7:42 the ventricles 7:43 and is a marker of ventricular distention or pressure, electrocardiogram which 7:50 may show 7:50 arrhythmia, echocardiogram to detect the ejection fraction as well as to look 7:56 for valvular problems 7:58 specifically in the presence of right-sided heart failure for example, chest x- 8:03 ray which 8:04 may show cardiomegaly, cardiac MRI to look for infiltrated diseases as well as 8:10 right 8:10 or left cardiac catheterization can be done. 8:15 Treatment of heart failure with preserved ejection fraction is divided into non 8:18 -pharmacological 8:19 and pharmacological, non-pharmacological approach includes reduced sodium 8:25 intake, stop alcohol, 8:26 stop smoking, encourage weight loss if overweight and exercise. 8:33 Pharmacological management of heart failure with preserved ejection fraction is 8:36 limited 8:36 as compared to heart failure with reduced ejection fraction. 8:41 Pharmacotherapy used include fruzamide, the loop diuretics, ACE inhibitors or 8:46 angiotensin 8:47 receptor blockers, spironolactone and SGLT2 inhibitors. 8:53 In summary, heart failure is a disorder in which the heart cannot pump blood to 8:56 the body. 8:58 Heart failure is classified into heart failure with reduced ejection fraction 9:01 and heart failure 9:02 with preserved ejection fraction. 9:05 Heart failure with preserved ejection fraction accounts for 50% of all heart 9:09 failure cases 9:10 and causes concentric ventricular remodeling. 9:13 It is associated with diastolic dysfunction. 9:16 The most common cause is hypertension. 9:19 Thank you for watching.