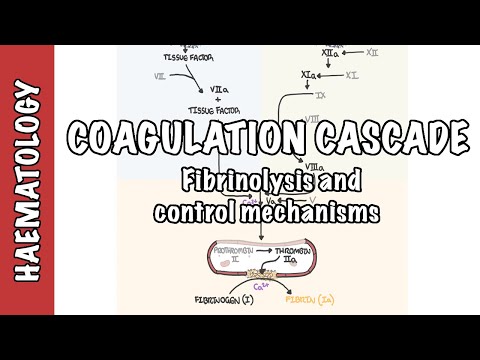
0:00 In this video we're going to talk about inflammation and inflammatory mediators 0:07 . 0:08 Inflammation is a body's immediate reaction to tissue injury or damage. 0:12 This damage can be caused by physical trauma, intense heat, irritating 0:17 chemicals and infections 0:19 by viruses, fungi or bacteria. 0:22 The cardinal signs of inflammation is edema which is swelling, pain, heat, ery 0:30 thema which 0:30 is redness and loss of function. 0:35 Although inflammation does cause pain and other problems, it is there to 0:38 protect you 0:39 and it does so by preventing the spread of infectious microorganisms and other 0:42 damaging 0:43 agents. 0:44 It destroys the pathogens and cell debris and prepares for repair of the damage 0:50 . 0:51 The inflammatory response begins with exposure of injured cells or dead cells 0:55 which release 0:56 damage associated molecular patterns and depending on the side of injury 1:01 pathogens and their 1:02 pathogen associated molecular patterns, the molecular patterns will trigger 1:09 inflammation. 1:10 The key players in the inflammatory response are mast cells, phagocytes in the 1:16 area and 1:17 in circulation including dendritic cells and macrophages, monocytes and neut 1:25 rophils also 1:25 known as polymorph nuclear leukocytes, endothelial cells around the site of 1:31 injury including 1:32 the blood vessels, platelets and four plasma protein systems including the clot 1:39 ting factors, 1:40 complement proteins, the kinin system and immunoglobulins which I have not 1:47 drawn here. 1:52 Once an injury occurs, inflammation involving all the key players that I talked 1:57 about will 1:58 occur. 1:59 Realistically everything happens at the same time but for simplicity we'll 2:03 create a story. 2:04 The inflammatory response occurs due to the help of inflammatory mediators 2:09 which can 2:10 be classified broadly into cell derived inflammatory mediators and plasma 2:16 derived inflammatory 2:17 mediators. 2:18 Let's focus on the cell derived inflammatory mediators first. 2:23 Injury to the tissue releases damage associated molecular patterns and pathogen 2:27 associated 2:28 molecular patterns. 2:30 Mast cells in the area detect this and release preformed granules containing 2:34 serotonin and 2:35 histamine. 2:37 Inflammation causes vasodilation, increasing blood flow to the area and 2:41 increases vascular 2:42 permeability allowing fluid, plasma proteins and cells to enter the site of 2:49 injury. 2:50 Surrounding phagocytes also release cytokines, another inflammatory mediator 2:54 including interleukin 2:55 1, interleukin 6 and TNF alpha. 2:59 Interleukin 1, interleukin 6 and TNF alpha promote the inflammatory response in 3:04 a number 3:04 of ways. 3:05 Firstly, it increases the expression of adhesion molecules on the surface of 3:10 endothelial cells 3:11 to allow recruitment of white blood cells including polymorph nuclear leuk 3:16 ocytes, called 3:17 neutrophils and monocytes which become macrophages when they enter the tissue. 3:26 Some of these cytokines also stimulate nerve endings triggering the pain 3:32 sensation. 3:33 drug cells and reciting immune cells also respond by synthesizing and releasing 3:39 inflammatory 3:40 mediators from the arachidonic acid metabolite and these include leukotrines 3:47 and prostaglandins. 3:49 Prostaglandins causes vasodilation, it stimulates nerve endings which causes 3:54 the pain sensation 3:55 and also causes fever. 3:58 Prostaglandins causes vasodilation and acts as a chemokine for chemotaxis, chem 4:04 okine is 4:04 an agent which attracts white blood cells so they know where the injury is, so 4:09 it attracts 4:10 macrophages and neutrophils which are necessary as they phagocytize pathogens 4:16 and cellular 4:17 debris to remove them. 4:20 The inflammatory mediators we talked about so far are cell derived inflammatory 4:25 mediators 4:25 which included the pre-formed granules such as histamine and also the newly 4:31 synthesized 4:32 mediators such as cytokines, prostaglandins and leukotrines. 4:39 The plasma-derived inflammatory mediators are mainly produced by the liver and 4:43 circulate 4:44 in plasma usually in an inactive form, they become activated during 4:50 inflammation. 4:52 These plasma-derived inflammatory mediators include the kinin system which 4:57 causes vasodilation, 4:59 it increases vascular permeability and stimulates nerve endings causing the 5:07 pain. 5:08 There is also the complement system proteins which are important for chemotaxis 5:13 again, 5:14 promoting phagocytic activity and creating what's called the membrane attack 5:19 complex 5:19 which essentially kills pathogens. 5:23 The inflammatory mediators promote inflammation allowing phagocytes to enter 5:28 the site of 5:29 injury and phagocytize pathogens and cellular debris. 5:38 Looking back at the cardinal signs of inflammation and their mechanisms, 5:42 swelling and edema occurs 5:44 in the area due to increase in vascular permeability and vasodilation. 5:50 Pain occurs due to stimulation of nerve endings, vasodilation increases blood 5:55 flow to the site 5:56 of injury causing redness, erythema and heat. 6:02 These different protein systems and different white blood cells and 6:05 inflammatory cells will 6:06 remain in the area until wound repair takes place. 6:11 When repair begins with hemostasis consisting of platelet plug formation and 6:16 clotting factors 6:18 triggering the coagulation cascade. 6:21 The end product is a fibroid mesh here in orange. 6:26 Fibroblasts and endothelial cells will then be recruited, they will proliferate 6:31 and wound 6:32 healing will take several weeks. 6:35 I will have a separate video on wound healing. 6:39 So in summary we talked about inflammation, the cardinal signs of inflammation 6:44 and inflammatory 6:45 mediators which can be classified as cell-derived inflammatory mediators and 6:50 plasma-derived inflammatory 6:51 mediators. 6:52 Thank you for watching.