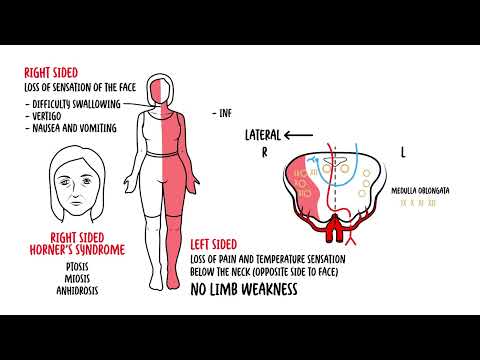
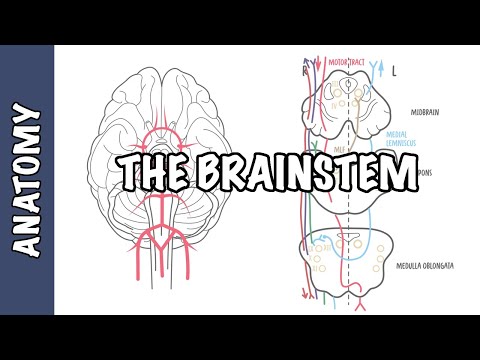
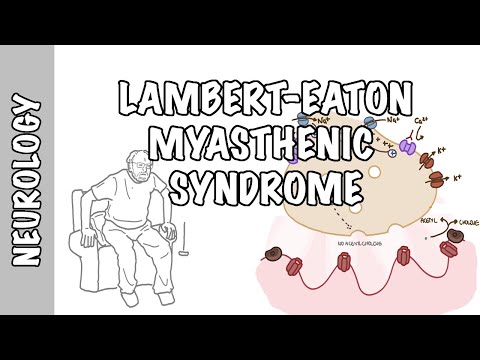
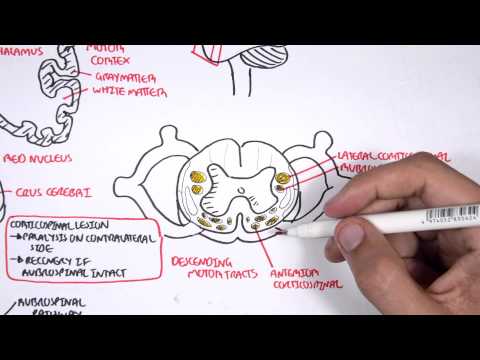
0:00 Hello, in this video, we're going to learn about midbrain syndromes. 0:13 This is a second part video to the midbrain anatomy video. 0:22 In order to talk about midbrain syndromes, we first need to revise the rules of 0:29 four for 0:29 the brainstem, which is a simplified method that is used to understand brain 0:35 stem anatomy 0:36 and brainstem vascular syndromes. 0:39 So the rules of four, as the name suggests, there are four rules. 0:46 And within each of these rules, it is all related to four, basically. 0:50 So the first rule of the rules of four is that there are four structures in the 0:57 midline 0:58 of the brainstem, beginning with M. And these are the motor pathways, or the 1:06 cortical spinal 1:07 tract, which passes the midline, the medial lemoniscus, the medial longitudinal 1:12 fasciculus 1:13 and the pathway, as well as the motor nuclei and cranial nerves, which are also 1:22 located 1:23 the nuclei in the midline. 1:27 The second rule of the rule of four is that there are four structures to the 1:34 side, or 1:35 lateral, beginning with S, so S for sides. 1:40 And these structures are the spinocerabella pathway, the spinothalamic pathway, 1:47 the sensory 1:48 nuclei of the fifth cranial nerve are located laterally, as well as the 1:55 sympathetic pathway. 1:57 The third rule of the rule of four is that there are four cranial nerves in the 2:06 medulla, 2:08 which is the bottom part of the brainstem. 2:10 There are four cranial nerves in the pons and four cranial nerves above the p 2:15 ons, two 2:16 in the midbrain and two above. 2:19 So again, above the pons, there are cranial nerves, one, two, three, and four, 2:25 cranial nerves 2:26 three and cranial nerves four are within the midbrain. 2:31 In the pons, there are cranial nerves five, six, seven, and eight, and in the 2:35 medulla there 2:36 are cranial nerves nine, ten, eleven, twelve. 2:42 The last rule, the fourth rule of the rule of four is that the four cranial 2:49 nerve nuclei 2:50 that are in the midline can be easily remembered by being divisible or that can 2:57 divide equally 2:59 into twelve, except one and two. 3:03 So the four cranial nerves I'm talking about that are in the midline and divide 3:07 equally 3:07 into twelve include cranial nerves three, cranial nerves four, six, and twelve. 3:16 Cranial nerves five, seven, nine, and eleven are in the lateral aspect of the 3:21 brainstem. 3:22 What makes this even more interesting is that the cranial nerves at the midline 3:29 , so three, 3:30 four, six, and twelve, are all motor nerves. 3:38 So now that we have revised the rule of fours of the brainstem, we can now use 3:45 what we have 3:46 learned to look at the midbrain syndromes. 3:51 And we're going to look at four midbrain syndromes in particular. 4:00 So in the first syndrome, let's talk about a case. 4:04 The case is of a woman that presents with sudden right-sided deplopia and pt 4:10 osis with 4:11 a down and out eye on that right side. 4:14 She also complains of left-sided weakness of her upper limb and lower limbs. 4:21 The signs and symptoms are caused by occlusion of a branch of the posterior 4:26 cerebral artery, 4:28 causing what is called Webis syndrome or Ventromedial Midbrain Syndrome. 4:36 In this case, the lesion is on the right side. 4:41 And what this results in is ipsilateral ocular motor nerve palsy. 4:46 So right-sided in this scenario, causing deplopia, ptosis, and the eye going 4:52 down and out. 4:54 It also causes right-paramidal motor tract lesion involvement in the midbrain. 5:00 And so this will result in contralateral hemiparesis, because remember, the 5:06 motor fibres actually 5:07 decasade in the medulla. 5:14 The second syndrome, again, a case of a man that presents with right-sided depl 5:21 opia and 5:21 ptosis and a down and out eye. 5:25 But this time, the man actually presents also with left-sided sensory changes, 5:30 specifically 5:31 vibration and proprioception loss, heals has left-sided hemiparesis and 5:38 associated ataxia. 5:43 This presentation is caused by a condition called Benedict syndrome. 5:50 Benedict syndrome occurs due to a lesion in the tegmentum of the midbrain, as 5:55 well as 5:55 the cerebellum. 5:57 The lesion can be due to infarction, hemorrhage, tumor or infiltrative 6:04 conditions such as tuberculosis. 6:10 It can result from occlusion of the posterior cerebral artery, or its 6:15 penetrating branches, 6:17 as well as the branches of the basilar artery. 6:22 In this case, the lesion is on the right side again. 6:27 Current textbooks vary considerably in the definition of the structures 6:31 involved with 6:32 this lesion. 6:35 What you get, again, with this right-sided, a Benedict syndrome, is ipsilateral 6:41 , so right-sided 6:42 oculomotor nerve palsy, causing deplopia, ptosis and the down and out eye. 6:49 The right lemaniscal tract in the midbrain will cause contralateral sensory 6:54 changes to 6:55 vibration and proprioception. 7:00 The red nucleus involvement will cause contralateral ataxia, specifically the 7:08 motor pathway. 7:10 The right pyramidal motor tract involvement in the midbrain will cause contral 7:15 ateral hemiparesis. 7:17 What I have not drawn here is that the superior cerebellar peduncle can also be 7:24 affected, 7:24 and this will cause ipsilateral sensory ataxia. 7:33 The third midbrain syndrome, without looking into a case, is called Claude 7:39 syndrome, and 7:40 it's used to describe ocular nerve palsy on the same side of the lesion with 7:44 contralateral 7:45 ataxia. 7:47 This is caused by lesions involving the third nerve fascicle itself. 7:57 Contralateral ataxia is due to involvement of the red nucleus, which is motor, 8:02 but again 8:03 in the same area, one can get ipsilateral ataxia, so on the same side due to 8:10 involvement 8:10 of the superior cerebellar peduncle. 8:14 This might get a bit confusing, but I hope that made sense. 8:20 The fourth and final midbrain syndrome, again we will look at a case. 8:26 Here you have a 75-year-old man who presents with impaired upward gaze, nystag 8:34 mus, and bilateral 8:36 lid retraction. 8:38 When you examine the old man, you notice that his pupils do not react to light, 8:45 so there 8:46 is impairment of light reaction, however, accommodation response is intact. 8:53 This, this last part specifically, where one does not respond to the light 8:58 reflex, but 8:59 can accommodate and pupils constrict, is known as argal Robertson pupil. 9:05 And all these signs and symptoms are due to a condition that can collectively 9:09 be called 9:10 paranoid syndrome, also known as the dorsal midbrain syndrome. 9:17 This condition results from injury to the mesenchyphallic tectum, the back of 9:22 the midbrain, causes 9:23 of paranoid syndrome, are brain tumours in the pineal or midbrain, demyel 9:29 ination within 9:30 the area or stroke of the upper brainstem. 9:35 Another manifestation of paranoid syndrome is convergence, retraction, nystag 9:40 mus. 9:40 And in order to understand this, you have to appreciate the diagram, which 9:45 shows you that 9:46 you have these supranuclear centres, which have nerve fibres that inhibit the 9:53 cranial 9:54 nerve 3 nucleus. 9:58 So damage of the midbrain supranuclear fibres, which normally inhibit the third 10:05 nerve nucleus, 10:07 essentially preventing activation of the extraocular muscles innervated by cran 10:11 ial nerve 3, will 10:13 be disrupted. 10:15 And therefore, these extraocular muscles, the medial superior and inferior rect 10:22 us muscles, 10:23 will have constant stimulation. 10:27 The eyes will retract, thanks to the superior and inferior rectus contraction. 10:35 And the eye will look medially due to medial rectus contraction. 10:39 And again, this is all because your cranial nerve 3 is active and there's no 10:43 inhibition 10:44 to that cranial nerve 3 nucleus. 10:50 Another manifestation is bilateral lid retraction. 10:54 And this is due to loss again of the supranuclear input to the third nerve 10:59 nucleus. 11:00 Without inhibitory effects of the supranuclear fibres at the posterior commiss 11:04 ure, the levato 11:06 papabras superioris receives constant stimulation via the oculomotor nerve. 11:10 And so you get lid retraction. 11:14 Finally, what you see in paranoid syndrome is Argyll Robertson pupil, also 11:20 known as light 11:21 near dissociation, where one can accommodate, but one does not respond to light 11:28 . 11:28 The pupils do not constrict to light. 11:30 And this, again, is due to injury or lesion to that posterior aspect or the 11:36 back of the 11:37 midbrain. 11:44 So in summary, in this video in particular, we talked about the rules of four 11:49 and midbrain 11:50 syndromes, specifically Weber's syndrome, Benedict's syndrome, Claude's 11:58 syndrome, and 11:59 lastly, Paranoid syndrome. 12:01 Thank you for watching.