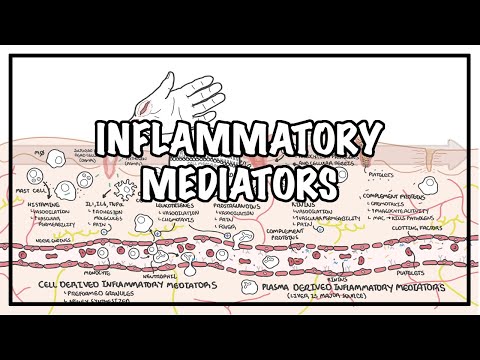
0:00 So you're going to biology and medicine videos, please make sure to subscribe 0:03 to our former 0:03 group for latest videos. Please be the first to know. Please like and he can 0:06 also ask questions. 0:07 Other questions are posted on interesting things including how it works. 0:09 You can also change the quality settings and the highest well prepared graphics 0:12 . 0:12 This video, we're going to look at inflammation as well as inflammatory 0:16 response. 0:17 So what is inflammation? Well, inflammation is the sum of the host defenses to 0:23 an 0:23 infectious or noxious stimuli. One of the major aims of inflammation is to 0:30 bring 0:30 defense cells, immune cells to the area of concern, as well as to inactivate or 0:37 destroy any 0:38 invaders, pathogens and to also begin repair in that area. Inflammation is 0:46 clinically denoted by 0:48 the suffix itis. So for example, dermatitis is inflammation of the skin. Ar 0:56 thritis is inflammation 0:59 of the joint. Let's look at inflammation in a bigger picture by looking at a 1:04 map and see what 1:05 happens when there is, for example, damage done to our skin and what sort of 1:10 inflammatory response 1:12 occurs. So inflammation. Here is the surface of our skin, a tissue, and we have 1:20 the sub mucosa 1:21 region underneath. Of course, below all this, we have blood vessels, many blood 1:26 vessels. 1:27 Here, I've only joined one blood vessel for simplicity. 1:30 However, of course, we actually have many blood vessels around the area 1:38 connecting to each other. 1:42 And then we also have lymphatic vessels here, which are important for immune 1:46 cells to move 1:47 around in, particularly the lymphocytes. The lymph vessels all connect to what 1:51 's called a lymph node 1:53 or other organs such as a spleen. Within the lymph node, if there is no 1:59 infection or infiltration 2:02 or inflammation, we have the naive cells, naive lymphocytes known as the B and 2:11 T cells. 2:11 Within the blood vessels, we have many types of cells and many types of plasma 2:19 proteins, etc. 2:20 We have erythrocytes, which are the red blood cells. We have monocytes. We have 2:27 neutrophils, 2:28 which are phagocytes. And because we're talking about inflammation, we have 2:34 also circulating in the blood vessel inflammatory mediators. It is important to 2:40 know that there are 2:40 two types of inflammatory mediators in general. The two types are the plasma 2:46 inflammatory mediators, 2:47 which means that these plasma are the ones that are circulating inflammatory 2:52 mediators. 2:53 And these are the cumbler proteins and the kinens. They are made by the liver, 2:59 and they circulate 3:00 with the blood vessel and are activated upon inflammation. The other type of 3:06 inflammatory 3:06 mediator is a cell derived inflammatory mediator, meaning that they come from 3:11 cells. And we'll talk 3:13 about them soon enough. Now, the cells that we find within the tissue or within 3:18 the surface of 3:19 skin or beneath the skin are what's known as mast cells. Mass cells contain 3:25 histamine granules. 3:26 And here we have another mast cell. Now, mast cells are really important cells 3:33 to promote inflammation, because histamine is a cell derived inflammatory medi 3:40 ator. 3:42 The other cells we find around this tissue are phagocytes, tissue macrophages, 3:50 for example, 3:51 as well as dendritic cells. Because we're talking about the skin, these dend 3:56 ritic cells are known 3:59 as Langerhand cells, and they're all around here. So now that we've got the 4:07 basics on the map here, 4:10 what happens during an injury? For example, a cut here. Well, blood will start 4:16 going out 4:17 because of the surrounding blood vessels. Now, it's important to note that 4:22 there's no step-by-step 4:24 process in inflammation. It's usually one of one happening with each other or 4:29 something like that. 4:31 So what can happen is that during this injury, a pathogen will infiltrate the 4:36 body and come into 4:37 the tissue. This pathogen, let's just say, is a bacteria, will trigger many 4:43 responses, 4:44 particularly by the surrounding cells, first of all. 4:46 So what happens is that this bacteria actually expresses certain proteins, 4:56 certain molecules on its surface, known as P-A-M-P. P-A-M-P is recognized by 5:05 the immune cells 5:08 They are recognized by the immune cells within the tissue, such as mast cells 5:11 and macrophages. 5:13 Once the mast cells recognize this pathogen, or recognizes that a pathogen has 5:19 infiltrated the 5:20 body, it will secrete the histamine. It has stored in the granules. Histamine, 5:27 when secreted, 5:28 will cause vasodilation and increase vascular permeability. 5:37 So here we have the blood vessels increasing in vascular permeability, 5:42 meaning the endothelial cells contract, allowing small gaps to form, as well as 5:48 the blood vessel 5:48 will dilate, vasodilation, which will increase blood flow, meaning that more 5:54 immune cells can come 5:56 inside the inflamed tissue. Because the blood vessels are permeable, these 6:04 immune cells in 6:04 the blood vessel can migrate to the inflamed tissue, or the site of 6:09 infiltration or injury. 6:11 The migration process, or immigration process, is known as diapodeses, and I 6:17 have a video on that. 6:18 Now what else could happen during this inflammation process? Well, the macroph 6:26 ages, 6:26 which recognize the P-A-M-P of the pathogen, will also secrete cytokines. 6:34 Cytokines is also an inflammatory mediator. The macrophages will secrete cytok 6:40 ines, 6:40 particularly cytokines TNF alpha, tumor necrosis factor alpha, and interleukin 6:48 1. 6:49 These cytokines will cause a local effect and a systemic effect, the local 6:56 effect being inflammation, 6:58 which is vasodilation, and increase in vascular permeability. The cytokines 7:04 will also trigger 7:06 or cause tissue repair by activating or stimulating fibroblast activity. 7:12 Now the cytokine systemic effect include a fever, so becoming hot, as well as 7:22 leukocytosis, 7:25 meaning the accumulation essentially of why blood cells are circulating within 7:29 the blood vessel, 7:30 and it usually happens during an inflammatory response. So anyway, the cytok 7:36 ines will essentially 7:37 also promote the immigration of these immune cells from the blood vessels into 7:43 the inflamed 7:44 tissue, such as a neutrophil and monocytes. When the monocytes actually move 7:50 from the blood 7:50 vessel into the tissue, the monocytes will become macrophages, so within the 7:56 blood vessel, 7:56 or while it's circulating, they are known as monocytes, but once they enter 8:00 tissues, 8:01 they are known as macrophages. So let's talk about repair too. As I mentioned, 8:08 the cytokine 8:09 TNF alpha into local one, the local effects it causes is repair. How does it do 8:20 this?