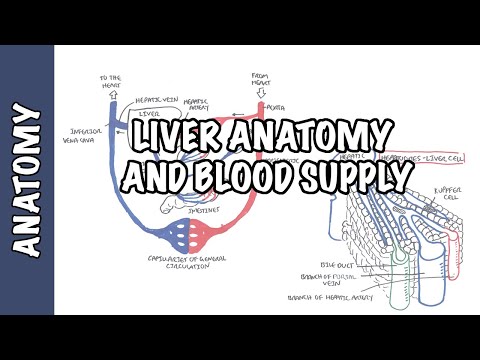
0:00 In this video we're going to talk about the complications and symptoms that can 0:19 be associated 0:20 with liver cirrhosis. 0:23 Liver cirrhosis is when we have fibrosis and starring of the liver. 0:27 Sleep liver cells is replaced with inflammatory cells and fibrous tissues. 0:32 This will lead to cell death of the liver cells. 0:36 The scarring and fibrosis and the cell death in a company in cirrhosis will 0:41 cause the liver 0:42 to shrink. 0:44 Before we delve into the complications associated with liver cirrhosis, we need 0:49 to familiarize 0:50 our cells with some organs that can be affected by liver cirrhosis. 0:57 So here is a human body and here is a liver suffering cirrhosis. 1:02 Notice the nodules. 1:04 Below the liver we have the gallbladder. 1:06 The liver and gallbladder will release bile from the common bile duct into the 1:11 small intestines 1:13 here. 1:15 The common bile duct will actually join with the duct coming from the pancreas 1:21 as well. 1:21 The bile is used to emulsify fat for absorption as well as many other things 1:26 and we won't 1:27 focus on the pancreas in this video. 1:30 Other organs that can be affected in cirrhosis include the esophagus that is 1:34 part of the digestive 1:36 tract and connects the mouth with the acidic stomach here. 1:40 The stomach then connects to the small intestines. 1:44 The small intestines will then connect to the larger intestines, the ascending 1:48 colon of 1:48 the larger intestines that is and then the ascending colon will join with the 1:52 transverse 1:53 and then the descending colon where feces will then be expelled from the rectum 2:00 here. 2:01 So what is important to know with all these digestive organs is that they are 2:06 supplied 2:07 with fresh oxygenated blood from the heart. 2:12 This red artery here coming from the heart. 2:15 This spleen is also an organ that is supplied by this fresh oxygenated blood 2:20 and is also 2:20 affected or damaged in cirrhosis. 2:26 So when all these organs have received this fresh blood from this red artery 2:33 then blood 2:34 will then leave through the veins and will leave from these digestive organs 2:40 via the vein 2:41 with deoxygenated blood and nutrients. 2:46 The veins leaving most of these digestive organs will not travel directly to 2:51 the heart 2:51 but will travel to the liver first. 2:55 So all the blood leaving these digestive organs will connect and travel into 3:01 the liver through 3:02 what is called the portal vein. 3:07 The liver not only receives this blood supply from all these digestive organs, 3:13 the intestines 3:14 stomach and spleen but also receives fresh oxygenated blood from the heart 3:18 through the 3:19 hepatic artery. 3:22 So the liver receives blood from two sources, hepatic artery, fresh oxygenated 3:26 blood and 3:27 the portal vein, which is blood supply coming from the digestive organs. 3:35 The liver will then process this and the blood will then travel out of the 3:38 liver through the 3:39 hepatic vein and connect to the inferior vena cava where it will return to the 3:44 heart. 3:45 Now if that did not make any sense to you, I have a video on liver blood supply 3:48 which 3:48 is very useful. 3:52 Other organs that can be affected by cirrhosis which I will talk about in this 3:55 video include 3:56 the lungs and the brain and the kidneys which I have not drawn yet. 4:03 Liver cirrhosis in general can cause two main problems which can then cause 4:08 other problems 4:09 but they are all associated together essentially. 4:13 These two problems are liver cirrhosis can cause is liver damage itself and 4:21 also portal 4:22 hyper tension. 4:25 Let us focus on portal hyper tension first as this can have a significant 4:30 impact on the 4:30 human body. 4:32 Remember the portal vein is the blood supply that travels through the liver 4:37 from the veins 4:38 coming out of other digestive organs. 4:41 So portal hyper tension is hypertension of this portal vein. 4:46 Portal hyper tension is where the fibrosis and scarring of the liver will lead 4:51 to the blocking 4:52 of blood flow through the liver and so we will have a portal vein bypass. 4:57 The pressure in the portal vein will increase because it cannot get through the 5:01 liver and 5:02 will result in blood flow going backwards essentially. 5:07 I hope that makes sense. 5:10 Let us zoom into the liver area and portal vein to understand more about the 5:13 complications 5:14 associated with portal hyper tension due to liver cirrhosis. 5:21 Let us review quickly the organs that can be affected with a portal hyper 5:24 tension first. 5:25 So here is the liver, the gallbladder, the esophagus connecting to the stomach, 5:29 stomach 5:29 to the small intestine, small intestine to the large intestine, I am only 5:33 drawing the 5:33 ascending and descending colon of the large intestine here and then the rectum 5:38 and finally 5:39 the spleen. 5:42 All the veins returning deoxygenated blood and nutrients from these organs will 5:48 flow through 5:49 the liver first before joining into the inferior vena cava. 5:53 And so here the gastric vein will join the portal vein, the spleen vein will 5:58 join the 5:59 portal vein, the intestine veins which are made up of predominantly, the 6:05 inferior mesenteric 6:06 vein will return blood from the descending large intestines and the superior 6:12 mesenteric 6:13 vein will return blood to the portal vein from connecting the portal vein from 6:18 the ascending 6:19 transverse and small intestines. 6:22 So all these veins will join to the portal vein which will not only provide the 6:28 liver 6:28 with deoxygenated blood but will provide the liver with nutrients for 6:33 processing because 6:34 the veins leaving the intestines for example are absorbing nutrients after we 6:43 eat. 6:43 The blood entering the liver will then leave the liver through the hepatic vein 6:47 and connect 6:47 with the inferior vena cava which will then return blood to the heart. 6:53 When we have liver cirrhosis it can cause blockage of blood flow through the 6:59 liver due 7:00 to fibrosis and liver scarring. 7:03 The blockage can really occur anywhere along the portal vein entering the liver 7:09 . 7:09 This will cause the, this will cause portal vein bypass. 7:13 The blood cannot go through because the pressure in the portal vein is 7:20 increasing causing blood 7:23 to flow backwards towards areas such as the stomach and esophagus. 7:28 When the blood flow, when the blood flows backwards towards the esophagus it 7:32 can cause 7:32 esophageal varices. 7:35 Asophageal varices is caused by portal hypertension. 7:39 When we have blocking of blood flow through the liver, through the portal vein, 7:44 and this 7:45 will result in increased pressure in the portal vein. 7:49 The increased pressure will cause blood to bypass and go backwards towards the 7:55 stomach 7:56 and esophagus. 7:57 So back towards the esophagus and gastric vein which will result in increase in 8:02 pressure 8:03 there. 8:04 The increase in pressure will cause varices, esophageal varices and we can have 8:09 bleeding 8:10 from these varices which can be very serious. 8:16 The splitting vein also normally carries blood to the liver via the portal vein 8:19 and so portal 8:20 hypertension can cause blood flow back to the spleen causing enlargement of the 8:26 spleen 8:26 also known as spleenomegalae. 8:30 So splitting vein joins to the portal vein. 8:34 Increase in pressure in the portal vein as in portal hypertension will cause 8:39 blood flow 8:40 bypass back to the spleen. 8:43 Spleen normally removes older red blood cells and white blood cells and plate 8:47 lets. 8:48 So a blocked blood flow from the spleen to the liver will cause accumulation of 8:54 cells 8:54 in the spleen and this will cause enlargement of the spleen, also known as sp 8:59 leenomegalae. 9:00 So what would this mean for the body? 9:05 Well, if all these red blood cells, white blood cells and platelets are 9:10 accumulating 9:11 in the liver and can't get out, if we would check the blood of this person 9:15 suffering from 9:16 liver cirrhosis, he would have thrombocytopenia, low platelet count which means 9:24 that there would 9:25 be insufficient clotting for the body and then he will have anemia which would 9:30 mean that 9:30 there's poor oxygen supply and he would have a nucopenia meaning that he would 9:36 have low 9:37 white blood cell count in the blood and this would mean that he'd probably be 9:41 more prone 9:41 to infection and all these there are low amounts of these cells because they're 9:48 all accumulating 9:49 in the liver because the blood can't really flow out properly remember. 9:55 Another problem due to the portal hypertension can coming where the veins 10:02 coming from the 10:03 rectum can't flow back out, this would lead to hemorrhoids, a condition known 10:09 as hemorrhoids. 10:10 So that's another condition for liver cirrhosis. 10:14 Now, portal hypertension due to cirrhosis can also cause other serious 10:21 complications 10:22 in chronic cases such as hepatic insulopathy. 10:26 Normally, ammonia from protein and amino acids metabolism is eliminated in bio 10:31 from the liver. 10:33 However, due to the bypass due to the portal hypertension, detoxification of 10:40 ammonia cannot 10:41 occur and so excess ammonia can then reach the brain causing hepatic insul 10:46 opathy, causing 10:48 loss of concentration, loss of memory, confusion, decreaseless, levels of 10:53 consciousness, coma, 10:55 and even death. 10:58 Another complication which is related to liver damage as well as portal 11:02 hypertension 11:03 is hepatic pulmonary syndrome. 11:06 Hepatic pulmonary syndrome is seen in about one third of cases of cirrhosis. 11:10 To understand what happens in this syndrome, we have to just recap about our 11:14 circulatory 11:15 system. 11:17 So remember, we have here the lungs and the heart. 11:21 The blood from the inferior vena cava, the superior vena cava enters the heart, 11:27 enters 11:27 the right atrium, and then exits out to be re-oxygenated in the lungs. 11:34 The re-oxyribable then comes back to the heart through the left atrium and then 11:39 be pumped 11:39 out of the heart to the rest of the body. 11:43 Now the pathophysiology of hepatic pulmonary syndrome is not fully understood, 11:48 but there 11:48 are a few ideas. 11:50 In advanced cirrhosis, the liver will start secreting hormones such as endothel 11:56 id-1 and 11:57 also cause common bowel death ligation. 12:00 Endothelid-1 is a vasoconstricture. 12:04 It causes smooth muscles to contract, for example. 12:07 However, in the absence of smooth muscles such as in the lung capillaries, it 12:13 will cause 12:14 vasodilation by releasing nitric oxide, NO. 12:19 Let's have a look. 12:20 So here, endothelid is traveling up to the heart and then into the lungs. 12:28 Let's zoom into the lungs to see how the endothelid causes nitric oxide to be 12:34 secreting. 12:35 So here we have sacs of alveoli. 12:38 The deoxygenated blood will come in to be reoxygenated by the alveoli and then 12:44 return 12:45 back to the heart. 12:48 Let's have a closer look at one alveolus. 12:52 The alveolus will essentially bring in oxygen and bring out carbon dioxide from 12:57 the lungs, 12:58 from our body. 13:00 First, we will look at a normal gas exchange. 13:04 So if here we have deoxygenated blood flow from the heart, it will come to the 13:10 alveolus 13:10 and receive oxygen, which will then bind to red blood cells and then flow back 13:15 to the 13:15 heart. 13:16 So we have fresh, oxidated blood. 13:19 What happens in advanced cirrhosis when we have endothelid-1 being secreted is 13:23 that it 13:24 will bind on the capillary cells and cause nitric oxide to be secreted, which 13:29 will cause 13:30 vasodilation and increase in blood flow. 13:34 This would mean that a lot of red blood cells flowing through won't be replen 13:38 ished with 13:38 oxygen, because there is too much flow and a buildup of pressure. 13:44 So it's uneven. 13:46 Common bile ductalization will actually cause glucose sites to start migrating 13:50 to the pulmonary 13:51 capillaries as well, which will further stimulate the secretion of nitric oxide 13:55 . 13:55 Therefore, we can say that hepatic pulmonary syndrome is induced by pulmonary 14:00 vasodilation 14:01 induced by nitric oxide. 14:04 This will cause an insufficient oxygen supply due to different pressures in the 14:07 capillaries 14:08 and alveolus. 14:10 This will also cause difficulty in breathing, and all this is due mainly by the 14:15 secretion 14:15 of hormones from a liver suffering advanced cirrhosis, such as the hormone 14:23 endothelid-1. 14:27 Now let's focus more on liver damage due to liver cirrhosis. 14:31 Hepatocarcinoma can occur because of uncontrolled multiplication of liver cells 14:36 for recovery 14:37 of lost cells. 14:39 Hepatocilocarcinoma is cancer of the liver. 14:43 Those include pain, swelling, hepatomegaly, and weight loss. 14:46 We would see a lot of cells dying in liver cirrhosis, and so there might be 14:54 uncontrolled 14:56 multiplication of liver cells, because of a homeostatic mechanism. 15:04 Complications with cirrhosis also include jaundice, yellowing of the skin, 15:07 which is pretty obvious. 15:11 This is because we might have intrahepatic obstruction of bowel flow from the 15:17 liver and 15:17 gallbladder into the swollen testines, and so bilirubin, which is supposed to 15:21 be part 15:22 of the bile being released in the swollen testines, will accumulate and cause 15:28 increased 15:28 bilirubin level in the plasma, and so yellowing of the skin. 15:33 While suffering from the liver cirrhosis might have pronounced yellowing of the 15:42 skin look. 15:43 I'm just drawing how the common bile duct here connects with the swollen test 15:47 ines to 15:47 show how blood flow is meant to release bile into the swollen testines, but an 15:52 obstruction 15:53 in the bile flow will result in jaundice. 15:57 Now the blood leaving the heart, the atrial blood supply, will supply fresh 16:03 oxygenated 16:04 blood to many organs. 16:06 For example, the inferior aorta will supply blood to organs, including that of 16:13 the kidneys 16:14 here. 16:15 We have two kidneys that is supplied with fresh oxygen blood. 16:19 The blood leaving the kidneys are the kidney veins, and they will connect with 16:23 the inferior 16:24 vena cava, which will then bring the deoxygen blood back to the heart. 16:29 It will not connect with the liver, it will just connect with the inferior vena 16:33 cava straight 16:34 away. 16:35 Now a complication that can occur due to liver damage caused by liver cirrhosis 16:40 , also a 16:40 syndrome is known as hepato renal syndrome. 16:48 There is actually no damage to the kidneys, but kidney perfusion is reduced, 16:53 the blood 16:53 flow is reduced. 16:55 Why would kidney perfusion be reduced? 16:57 Well an example is because of insufficient blood supply to the kidneys. 17:03 To see what happens, we would first try to see why we would have insufficient 17:06 blood supply 17:07 to the kidneys. 17:09 It's actually all portal hypertension's fault, or obstruction of blood flow 17:13 through 17:14 the liver, somewhere. 17:15 Because remember, we have all this blood flowing from all these organs back to 17:20 the liver. 17:21 So if we have an obstruction of the portal hypertension, or portal hypertension 17:24 , the 17:25 blood will flow backwards and cause increase in pressure in different tissues 17:29 around the 17:30 abdominal region. 17:33 This can cause a condition known as aside, when we have fluid leaking out of 17:38 the capillaries 17:39 due to the buildup of pressure in the portal vein. 17:42 This will cause blood to flow backwards, causing a buildup of pressure 17:47 elsewhere, and then 17:48 fluid will leak out into the abdominal cavity. 17:52 This will cause a stomach to look very big, something like a demon of the 17:56 stomach. 17:57 And this is very dangerous as infections can easily occur in people with aside. 18:03 So because all the fluid is accumulating in the stomach, and the fluid is not 18:07 returning 18:08 properly to the heart, the heart will think that it does not have enough blood 18:14 supply, 18:15 type of lemium, and so will induce some homostatic mechanism to cause an 18:20 increase in fluid volume. 18:23 There will be arterial vasodilation, not atrial vasodilation, as I wrote here. 18:30 There will be arterial systemic vasodilation to try to increase blood flow to 18:36 the organs. 18:37 The kidneys, because it is not receiving enough blood, enough fluid, it will 18:41 activate the renin 18:43 angiotensin-outosterone system. 18:46 This will stimulate the reabsorption of water and sodium from the kidneys, 18:50 which will therefore 18:51 increase water and sodium levels in the body to compensate for this lack of 18:58 blood supply. 19:00 So hepaterinol syndrome is when we have no actual damage to the kidneys, but 19:04 due to hypovolemia, 19:06 low fluid volume in the blood, the kidneys will activate the renin angiotensin- 19:11 outosterone 19:12 system, which will cause an increase in sodium and water reabsorption. 19:18 But the thing is, we don't really need any more water and sodium, because we 19:21 already 19:22 have heaps, it's just water and sodium are in the abdominal cavity, or just 19:26 aren't flowing 19:27 through the liver properly. 19:30 This will then lead to more complications, such as edema. 19:34 The increase in water volume will cause swelling of the hands and ankles defeat 19:42 . 19:43 I hope that made sense. 19:44 Now itching is another symptom of liver cirrhosis, because of the high levels 19:48 of uric acid in 19:49 the skin, which can't be cleared by the liver. 19:55 I hope you enjoyed this video on liver cirrhosis, it might have been boring, 19:58 and there might 19:59 have been some mistakes, but it's interesting to know how all these 20:02 complications do connect 20:03 with each other. Thank you.