Antiphospholipid Syndrome (APS)
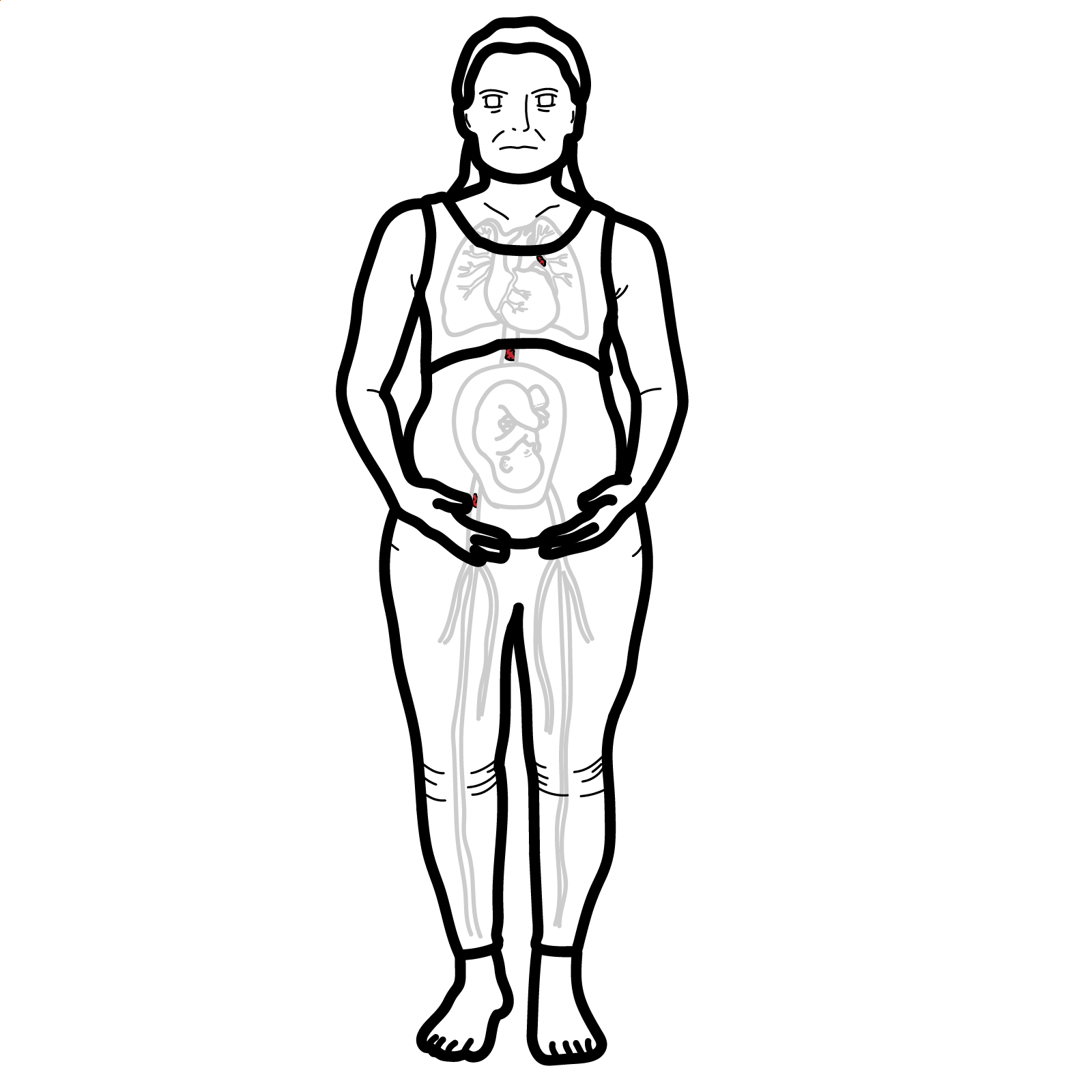
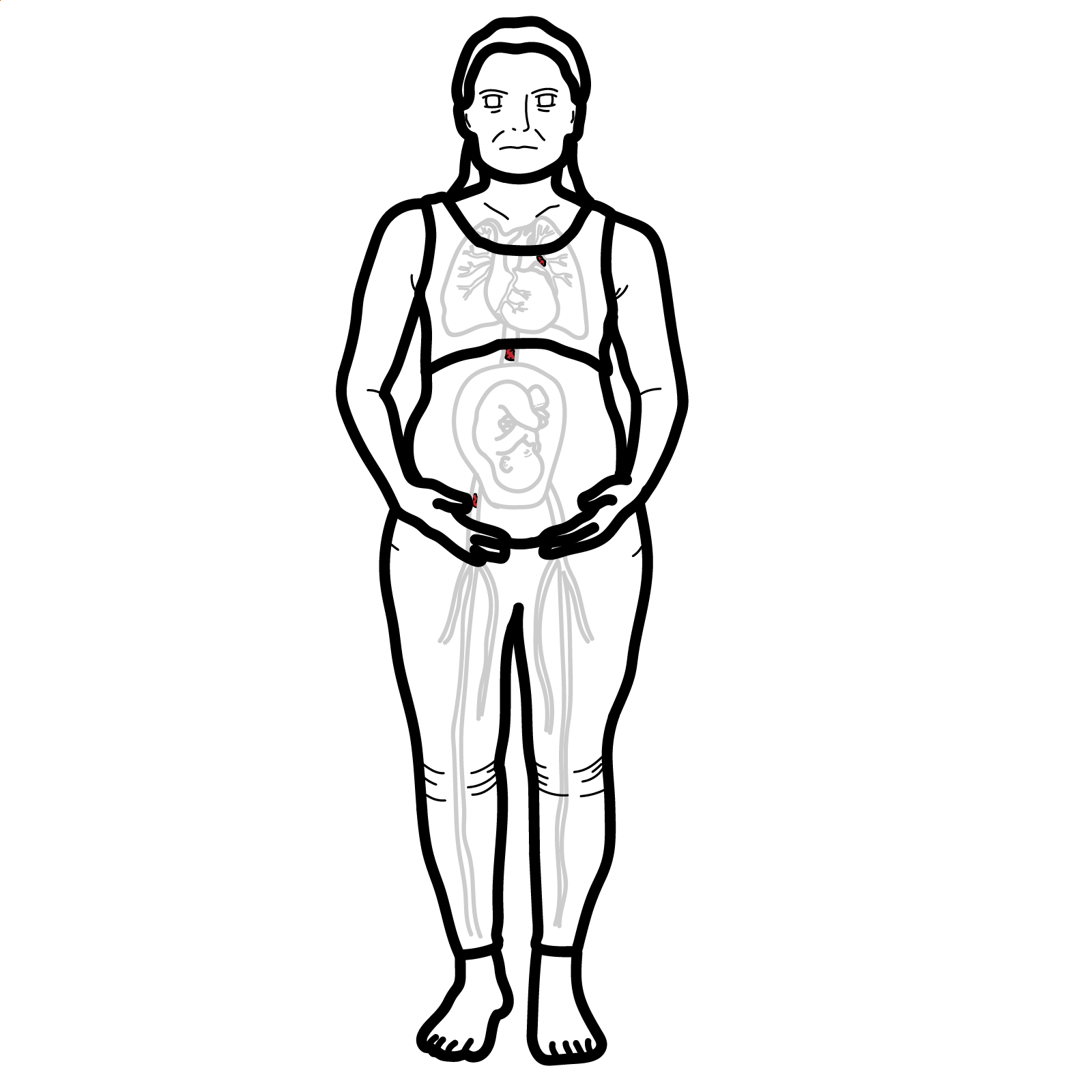
Antiphospholipid Syndrome (APS) is an acquired autoimmune thrombophilia characterized by recurrent venous or arterial thromboses and/or pregnancy morbidity in the presence of persistent antiphospholipid antibodies (aPL). APS may occur as a primary condition or secondary to systemic lupus erythematosus (SLE). Prevalence of aPL in the general population is ~2%, but true APS is rare (~40–50 per 100,000); female predominance (F:M = 3:1). APS is a leading cause of recurrent pregnancy loss and unexplained thrombosis in young individuals.
Antiphospholipid antibodies (aPL): Autoantibodies directed against phospholipid-binding proteins such as β2-glycoprotein I or cardiolipin.
Lupus anticoagulant (LA): A misnomer; it causes in vitro prolongation of clotting tests but is prothrombotic in vivo.
Thrombophilia: A disorder that increases the risk of thrombosis.
Catastrophic APS (CAPS): A rare and life-threatening form of APS with multiorgan thrombosis over days.
Steps in thrombosis
Three major contributors to thrombosis:
Despite prolonged aPTT on labs, APS is prothrombotic due to antibody-mediated vascular injury.
| System | Manifestations |
| Vascular | DVT, PE, stroke, TIA, retinal thrombosis |
| Obstetric | Recurrent miscarriage (>10 weeks), fetal death, preeclampsia, IUGR |
| Cardiac | Libman-Sacks endocarditis, valvular thickening |
| Hematological | Thrombocytopenia |
| Dermatologic | Livedo reticularis, ulcers |
| Neurological | Seizures, cognitive dysfunction, chorea |
| Renal | Thrombotic microangiopathy, hypertension |
| Catastrophic APS | Rapid multiorgan thromboses, DIC-like picture |
Suspect APS in young patients with unprovoked thrombosis, especially arterial or recurrent pregnancy loss.
2023 ACR/EULAR antiphospholipid syndrome classification criteria
| Domain | Feature / Event | Weighted Points |
| Entry Criterion | At least one positive aPL test (LA, moderate/high‐titer aCL or anti‑β2GPI IgG/IgM) within 3 years of clinical event | ★ Required before scoring |
| Clinical Domains (≥3 pts) | ||
| Macrovascular Venous Thrombosis | VTE with high-risk profile | 1 |
| VTE without high-risk features | 3 | |
| Macrovascular Arterial Thrombosis | Arterial event with CVD risk | 2 |
| Arterial event without CVD risk | 4 | |
| Microvascular Thrombosis | Suspected lesion (e.g. livedo, nephropathy, pulmonary hemorrhage) | 2 |
| Established pathology | 5 | |
| Obstetric Morbidity | ≥3 consecutive early losses (<10 weeks) | 1 |
| Fetal death (10–33 weeks) without pre‑eclampsia or placental insufficiency | 3 | |
| Fetal death with pre‑eclampsia or placental insufficiency <34 weeks (± fetal death) | 3 | |
| Fetal death with both pre‑eclampsia & placental insufficiency <34 weeks | 4 | |
| Cardiac Valve Disease | Valve thickening (non-infectious) | 2 |
| Valve vegetation (non-infectious) | 4 | |
| Haematologic Manifestation | Thrombocytopenia (20–130 × 10⁹/L) | 2 |
| Laboratory Domains (≥3 pts) | ||
| Lupus Anticoagulant (functional assay) | Positive (persistent) | 5 |
| aCL or anti‑β2GPI antibodies (ELISA) | Moderate‑titer IgM or IgG (40‑79 U) | 1 |
| Moderate IgG only | 4 | |
| High‑titer IgG and/or anti‑β2GPI (≥80 U) | 5 | |
| High‑titer IgG in both aCL and anti‑β2GPI | 7 | |
| Antibody | Description & Clinical Relevance |
| Anticardiolipin Antibodies (IgG or IgM) | • Target cardiolipin, a negatively charged phospholipid located on mitochondrial membranes. • May appear transiently at low levels in response to infections, malignancy, or autoimmune conditions—not always pathogenic. • IgG subtype is more strongly associated with thrombotic risk than IgM. |
| Anti-beta2-glycoprotein I Antibodies (IgG or IgM) | • Target beta2-glycoprotein I, a plasma protein that inhibits platelet aggregation and regulates the coagulation cascade. • IgG antibodies correlate more closely with thrombotic events. • IgM antibodies have lower clinical significance. |
| Lupus Anticoagulant | • Refers to a functional group of antibodies (not a single entity) that interfere with phospholipid-dependent clotting assays. • Most predictive of thrombotic and obstetric complications in APS. • A persistently positive lupus anticoagulant carries higher clinical risk than anticardiolipin or anti-beta2GPI antibodies. |
Differential Diagnoses
| Condition | Distinguishing Features |
| Inherited thrombophilia | No aPL; family history; no obstetric loss |
| DIC | Consumptive coagulopathy; ↓ fibrinogen |
| TTP | Microangiopathy, neurologic findings, ADAMTS13 deficiency |
| SLE alone | Multisystem inflammation but may coexist with APS |
Treatment (not obstetrics)
Treatment (obstetrics)
Avoid Direct Oral Anticoagulants (DOACs) in triple-positive patients or arterial events (↑ recurrence risk).
Long-term warfarin is mainstay for thrombotic APS; DOACs are NOT equivalent in high-risk APS.
Complications
Poor Prognostic Factors:

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion