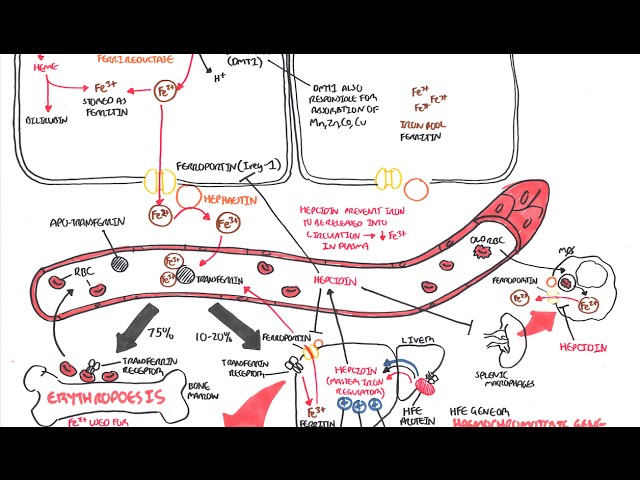
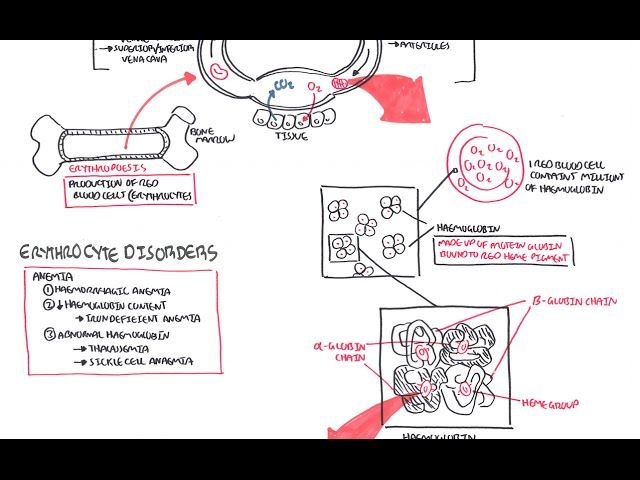
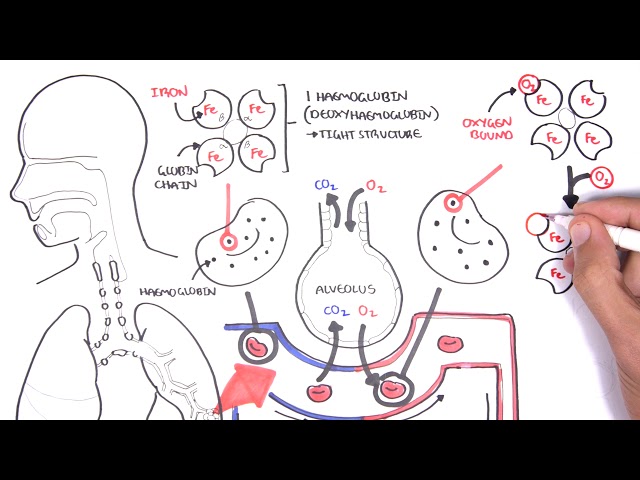
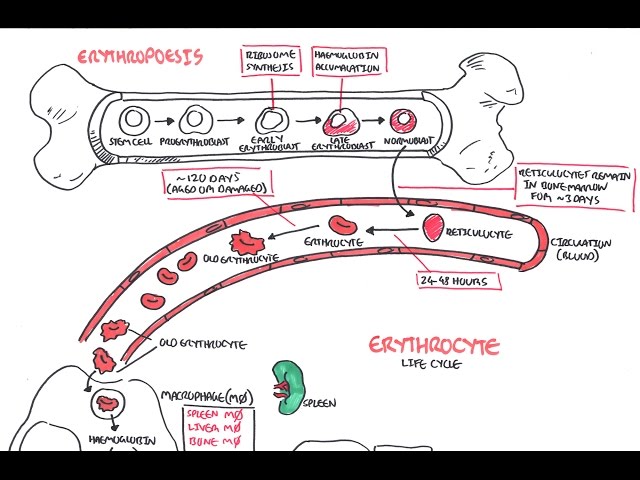
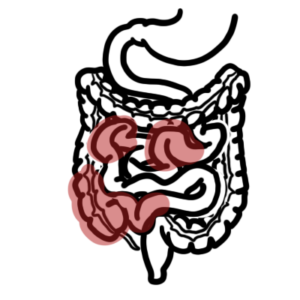
0:00 Hello, in this video, we're going to talk about hemochromatosis. 0:10 Hemo means blood, chromat means color, and osis means disease. 0:14 So it's essentially a condition that causes changing of color in the blood, but 0:20 not only 0:21 the blood, also the tissues and organs of your body. 0:25 Hemochromatosis is essentially when you have too much iron in your body. 0:29 You have iron overload, and there are many causes. 0:33 You can have primary, which is the hereditary hemochromatosis or secondary hem 0:38 ochromatosis. 0:39 The normal iron content of the body is about three to four grams. 0:44 It exists in four main forms. 0:47 The first is iron is found as storage in the forms of ferritin or hemocidarin. 0:54 Here you can see it's in a ferric iron state, and this is how I'm going to 0:59 depict it. 1:00 You can also find iron bound to transference, which is the transportation of 1:05 iron in the 1:05 plasma. 1:08 Finally, you can also find iron in hemoglobin, which is where the majority of 1:19 it is found, 1:20 and hemoglobin is important because it carries the oxygen around our body. 1:25 Iron can also be found in other proteins and enzymes within the body. 1:32 We get iron from certain foods and vegetables, and when we eat, it goes into 1:38 our stomach, 1:39 and it actually gets absorbed in the area of the small intestine called the du 1:44 odenum. 1:44 Here iron is absorbed via a transporter on the apical surface of the enter 1:49 ocytes called 1:50 DMT1. 1:52 From here, iron can either be stored as ferritin again, or it can be re-absor 1:59 bed into circulation 2:01 via feroportin, the orange transporter here, a very important transporter. 2:09 Once iron is in the circulation, it is bound to the transporter called transfer 2:16 in, and 2:17 remember, transferin is the transporter that carries iron all around the body. 2:22 From here, iron can be brought into the bone marrow where we make more red 2:29 blood cells, 2:30 so iron stimulates erythropoasis, and from here you get new red blood cells. 2:38 Well eventually, about 120 days or so, the red blood cells die and they get 2:43 essentially 2:43 destroyed by the reticular endothelial system, and essentially a recycling 2:49 process happens. 2:50 The iron is once again released into circulation and bound to transferin. 2:56 It's really important to know that the majority of the iron that we take in 3:02 gets put into erythropoasis, 3:05 we need more red blood cell. 3:09 The remainder goes into other tissues and organs, but mainly so, the liver. 3:15 Here the liver can also store iron as ferritin. 3:21 The liver also produces this important protein called hepsidin. 3:28 You can think of hepsidin as the main regulator of iron metabolism, as well as 3:33 iron absorption 3:34 and regulation. 3:37 Essentially hepsidin's goal is to lower serum iron. 3:43 Hepsidin gets stimulated or released when there's a lot of iron in storage. 3:48 Secondly, inflammation can also promote the release of hepsidin as well. 3:56 Hepsidin's goal is to lower serum iron, and it does this through a number of 4:01 ways, but 4:02 the most important way, is that it inhibits feroportin. 4:06 It essentially promotes the destruction of feroportin, both in the enterocytes, 4:11 as well 4:11 as in the liver, as well as in the red blood cells. 4:15 It inhibits the release of iron into circulation, thus lowering serum iron 4:25 levels. 4:26 Now I would like to talk about the different causes of iron overload or hemoch 4:32 romatosis. 4:33 Firstly, when someone eats too much iron, this can cause iron overload, but you 4:40 'd have 4:40 to eat a lot for it to cause any significant complications. 4:45 Secondly, you can have mutations in certain transporters, such as feroportin, 4:52 and when 4:53 you have mutation feroportin, what happens is, is that you can have excess fer 4:59 oportin, 5:00 and when you have excess feroportin, all this iron can get into circulation. 5:05 Another cause of hereditary hemochromatosis is one affecting a gene called the 5:11 HFE gene 5:11 found on chromosome 6. 5:15 The genes affected include, specifically, mutations in the C2A2Y or the H6-3D. 5:25 This is the hereditary hemochromatosis, as we know. 5:29 The exact mechanism of how it causes hemochromatosis is not well known, but it 5:33 's known that it 5:34 also reduces hepsidin, and because hepsidin is reduced, it means that there is 5:41 no inhibition 5:43 of feroportin, so you have feroportin activated, releasing all this iron into 5:49 circulation, 5:50 causing iron overload. 5:53 Other causes of hemochromatosis include any sort of liver disease, chronic 5:59 liver disease, 6:01 be it from alcohol, non-alcoholic fatty liver disease. 6:05 These cause, for whatever reason, which is incompletely understood, it also 6:10 reduces hepsidin, 6:11 again, reduction hepsidin means that you cannot inhibit or stop feroportin from 6:21 working. 6:22 Another cause of hemochromatosis, which is secondary hemochromatosis, include 6:26 blood disorders, 6:27 such as thalassemia major or intermediate, as well as cideroblastic anemia. 6:34 Essentially what happens here is that when you have this anemia, it obviously 6:37 tries to 6:37 stimulate proper erythropoiesis, but essentially what you get is ineffective 6:43 erythropoiesis, 6:44 which leads to suppression of hepsidin. 6:53 Another cause of iron overload includes transfusional overload. 6:58 What I mean by this is that it's either iron transfusions for a person or red 7:04 blood cell 7:05 transfusions, such as for those who have thalassemia or myelodysplastic 7:11 syndrome or a plastic 7:12 anemia. 7:14 When you give someone red blood cells, they also contain iron. 7:17 Because they contain iron, you can cause secondary iron overload. 7:26 We looked at the different causes of iron overload. 7:30 When you have so much iron in circulation, the plasma iron binding protein, the 7:35 transporter 7:36 called transferin, becomes saturated. 7:40 When this happens, iron begins binding to other things, such as albumin, cit 7:46 rate, acetate. 7:48 This iron is referred to non-transferin-bound iron. 7:52 When this happens, cells will take up this non-transferin-bound iron into the 7:58 liver, for 7:59 example, the heart, the pituitary glands, the joints, the pancreas, as well as 8:09 the gonads. 8:11 And here they undergo biochemical reactions, which creates reactive oxygen 8:16 species, which 8:17 in turn causes tissue damage, inflammation, and fibrosis. 8:22 So for example, in the liver, it can cause cirrhosis. 8:28 As well, it increases the risk of hepatocellular carcinoma. 8:32 In the heart, it can cause restrictive or dilated cardiomyopathy, as well as 8:40 arrhythmia. 8:42 In the joints, it causes arthritis. 8:47 In the pituitary glands, when you have iron depositing here, it can cause 8:51 secondary hypothyroidism 8:53 or secondary hypogonadism. 8:58 In the pancreas, the deposition of iron can cause diabetes myelitis. 9:05 In the gonads, it can cause testicular atrophy, amongst many other things. 9:10 Further, one of the most earliest sign of hemochromatosis is bronzing of the 9:14 skin, or 9:15 pigmentation of the skin, due to increase in melanin deposition, as well as 9:22 iron. 9:22 And I want to highlight three main things here. 9:25 And I want you to remember that the triad of cirrhosis, diabetes, and skin pig 9:33 mentation 9:34 should remind you of hemochromatosis. 9:42 The diagnosis of iron overload, or hemochromatosis, include one, when you have 9:47 elevation of serum 9:48 plasma, a ferritin. 9:50 Two, when you have evidence of iron overload in the MRI, of the liver, or the 9:55 heart, for 9:56 example, something not commonly used now is evidence of iron overload on tissue 10:02 biopsy, 10:03 and this requires iron staining. 10:05 You can also diagnose it when you remove iron with a course of therapeutic phle 10:10 botomy, and 10:10 this will result in normalization of the ferritin levels. 10:16 In terms of treatment of hemochromatosis, the major treatments for iron 10:22 overload is phlebotomy, 10:24 essentially removing the blood, because when you remove blood, you're taking 10:27 iron with 10:28 it. 10:29 However, if someone already has anemia, which is low red blood cells, you 10:33 wouldn't want 10:33 to take out more blood, and so an alternative is using iron-keelating agents, 10:39 which also 10:40 reduces serum iron levels. 10:43 Thank you for watching. 10:44 I hope you enjoyed this video. 10:46 �