Caplan Syndrome
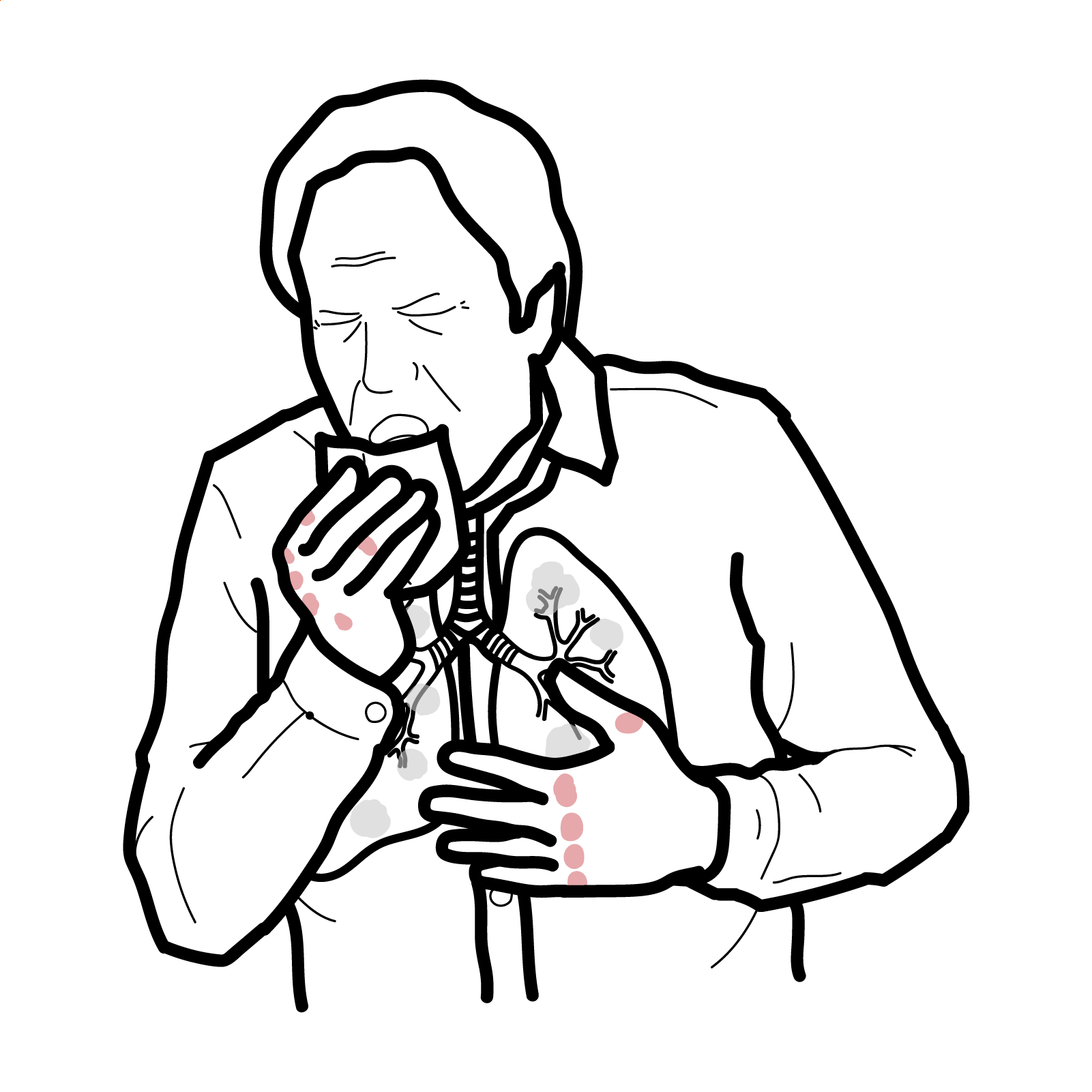
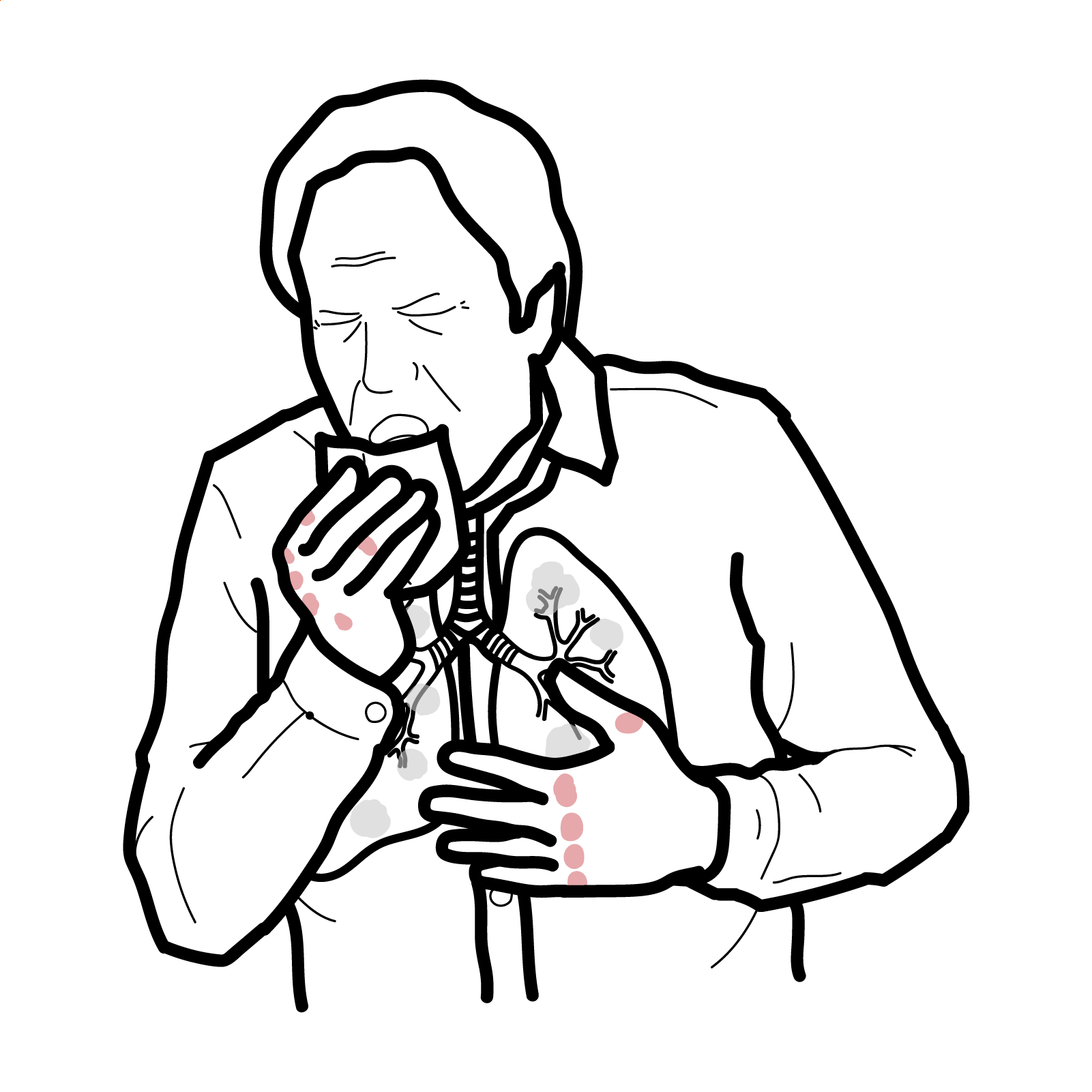
Caplan syndrome, also known as rheumatoid pneumoconiosis, is a rare condition seen in patients with rheumatoid arthritis (RA) who have had occupational exposure to inhaled dust, particularly coal dust or silica. It is characterised by multiple, rounded pulmonary nodules and underlying pneumoconiosis. It primarily affects middle-aged male coal workers and is now rare in developed countries due to improved occupational safety. Nodules are typically asymptomatic but may be associated with cough, dyspnoea, or constitutional symptoms in active RA.
Rheumatoid arthritis (RA): Chronic autoimmune inflammatory disorder targeting synovial joints with systemic manifestations.
Pneumoconiosis: Lung disease caused by inhalation of dust particles (e.g., coal, silica), leading to fibrosis.
Caplan nodules: Rounded, necrobiotic lung nodules in patients with RA and dust exposure.
Silicosis: Progressive lung disease caused by inhalation of silica dust, often seen in mining or construction workers.
Caplan syndrome occurs only in patients with RA + dust exposure — both are required1.
Caplan syndrome differs from simple pneumoconiosis by the presence of RA and immunologically driven nodules.
No formal diagnostic criteria
• Known RA
• History of relevant dust exposure
• Radiographic findings: multiple round nodules (0.5–5 cm), typically in upper lobes
Investigations
• Chest X-ray or CT: rounded peripheral nodules, usually bilateral and upper lobe predominant
• Pulmonary function tests: may show restrictive defect or normal
• Serology: positive RF or anti-CCP
• BAL (bronchoalveolar lavage) or biopsy if nodules are atypical or rapidly enlarging (to exclude malignancy or infection)
• ESR/CRP: may be elevated with RA activity
Differential diagnoses
| Condition | Key Features | Differentiating Points |
| Silicosis | Nodules + exposure | No RA, no serology positivity |
| Sarcoidosis | Bilateral hilar lymphadenopathy | Non-caseating granulomas, systemic involvement |
| Lung cancer | Solitary nodule or mass | Irregular margins, smoking history |
| Rheumatoid lung disease | Interstitial pattern | Diffuse fibrosis, not rounded nodules |
Triad: Rheumatoid arthritis, Occupational dust exposure and Pulmonary nodules on imaging.
RA management:
Avoid further dust exposure
Symptomatic pulmonary care:
Surgical intervention: rarely needed; biopsy may be performed if diagnosis unclearMonitor for superimposed infection, nodule growth, malignancy.
Withdrawal from exposure is crucial — lung nodules often stabilise or regress once exposure ceases2.
• Nodule cavitation, rupture
• Secondary infection
• Misdiagnosis as TB or malignancy
• Interstitial lung disease (in advanced cases)
• Prognosis generally good if exposure is discontinued and RA controlled

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion