Felty Syndrome
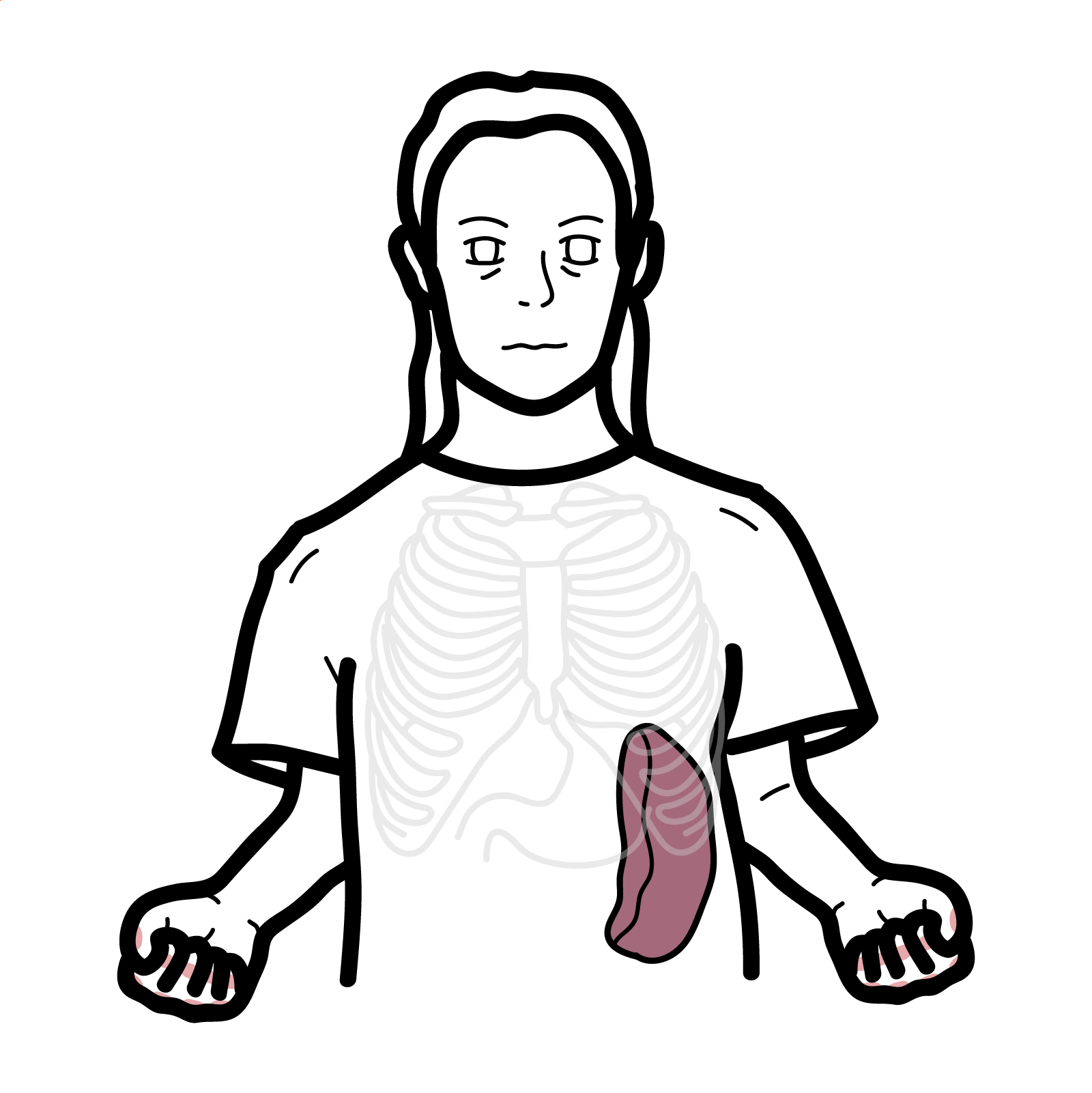
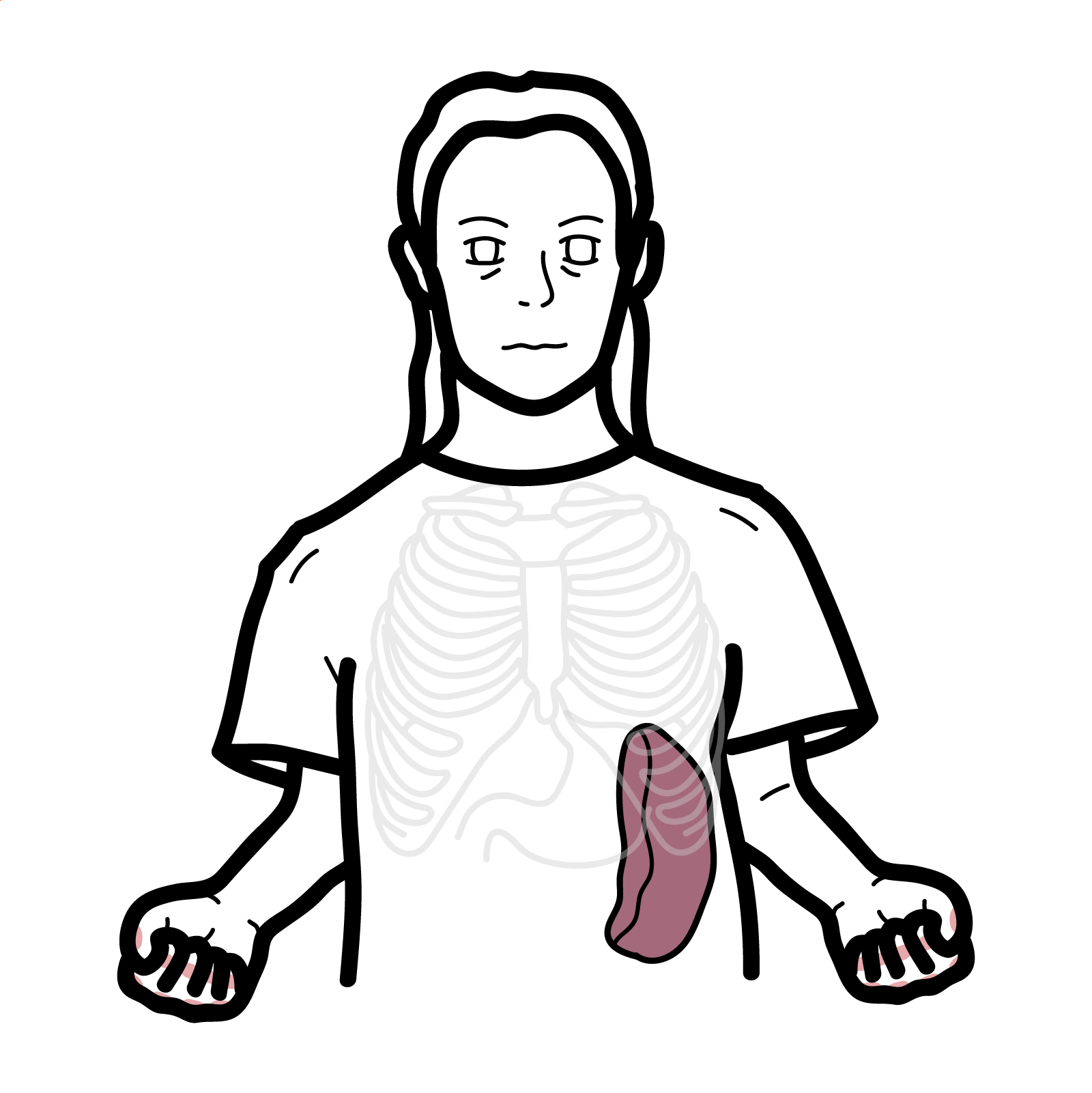
Felty syndrome is a rare but serious extra-articular manifestation of long-standing, seropositive rheumatoid arthritis (RA), characterized by the classic triad of RA, splenomegaly, and neutropenia. It was first described in 1924 by the US-American physician Augustus Roi Felty. It most commonly occurs after at least 10 years of poorly controlled RA and is associated with severe joint damage and extra-articular features. It predominantly affects middle-aged Caucasian women and may signal more aggressive disease. Occurs in <1% of patients with RA.
Rheumatoid arthritis: A chronic autoimmune inflammatory polyarthritis primarily affecting synovial joints, with systemic manifestations.
Splenomegaly: Enlargement of the spleen, commonly due to hyperplasia of lymphoid tissue or congestion.
Neutropenia: An absolute neutrophil count (ANC) <1500/μL, increasing the risk of infection.
Extra-articular RA: Manifestations of RA affecting organs outside the joints, including skin, lungs, and bone marrow.
Aetiology
• Autoimmune process driven by chronic RA
• T-cell mediated destruction or peripheral sequestration of neutrophils
• Immune complex deposition in spleen
Risk Factors
• Long-standing RA (>10 years)
• Seropositive RA (RF and anti-CCP positive)
• Caucasian ethnicity
• Female sex (F:M ratio ~3:1)
• Presence of HLA-DR4 allele
>90% of patients with Felty syndrome are rheumatoid factor (RF) positive1.
Always consider Felty syndrome in patients with long-standing RA and unexplained recurrent infections.
Triad: Rheumatoid arthritis, Splenomegaly, Neutropenia
Diagnostic criteria (clinical diagnosis based on classic triad; no universal criteria established):
• Known seropositive RA
• Absolute neutrophil count <2000/μL
• Splenomegaly on imaging or examination
Investigations
• FBC: neutropenia, anemia, thrombocytopenia
• ESR/CRP: elevated in active RA
• RF and anti-CCP: usually positive
• ANA: may be positive
• LFTs: mild elevation possible
• Bone marrow biopsy: to exclude myelodysplastic syndrome
• Imaging: ultrasound/CT showing splenomegaly
• Synovial fluid analysis (if effusion present)
Differential diagnoses
| Condition | Key Features | Differentiating Points |
| Large granular lymphocytic (LGL) leukemia | Neutropenia + splenomegaly | Clonal T-cells on flow cytometry |
| SLE | Cytopenias, autoantibodies | Malar rash, renal, serositis; lacks erosive arthritis |
| Myelodysplastic syndrome | Pancytopenia, dysplasia | Bone marrow biopsy shows dysplastic changes |
| Hypersplenism | Cytopenias with splenomegaly | No RA or autoantibodies |
Always rule out LGL leukemia with flow cytometry when neutropenia is present with RA2.
Control RA inflammation:
Treat neutropenia:
Manage infections promptly
Prognosis depends on recurrent infection. Splenectomy may normalise Neutrophil count in 50-80 of refractory cases.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion