Overview
One of the most common biochemical abnormalities in the body is elevated calcium levels in the blood, which is referred to as hypercalcaemia . Primary hyperparathyroidism and malignancy are the two most common causes of increased serum calcium levels. The presence of high or not adequately suppressed serum parathyroid hormone levels should point the diagnosis towards hypercalcaemia of parathyroid origins. Severe hypercalcaemia requires admission to hospital and treatment with aggressive intravenous hydration and bisphosphonates along with treatment of the underlying disease.
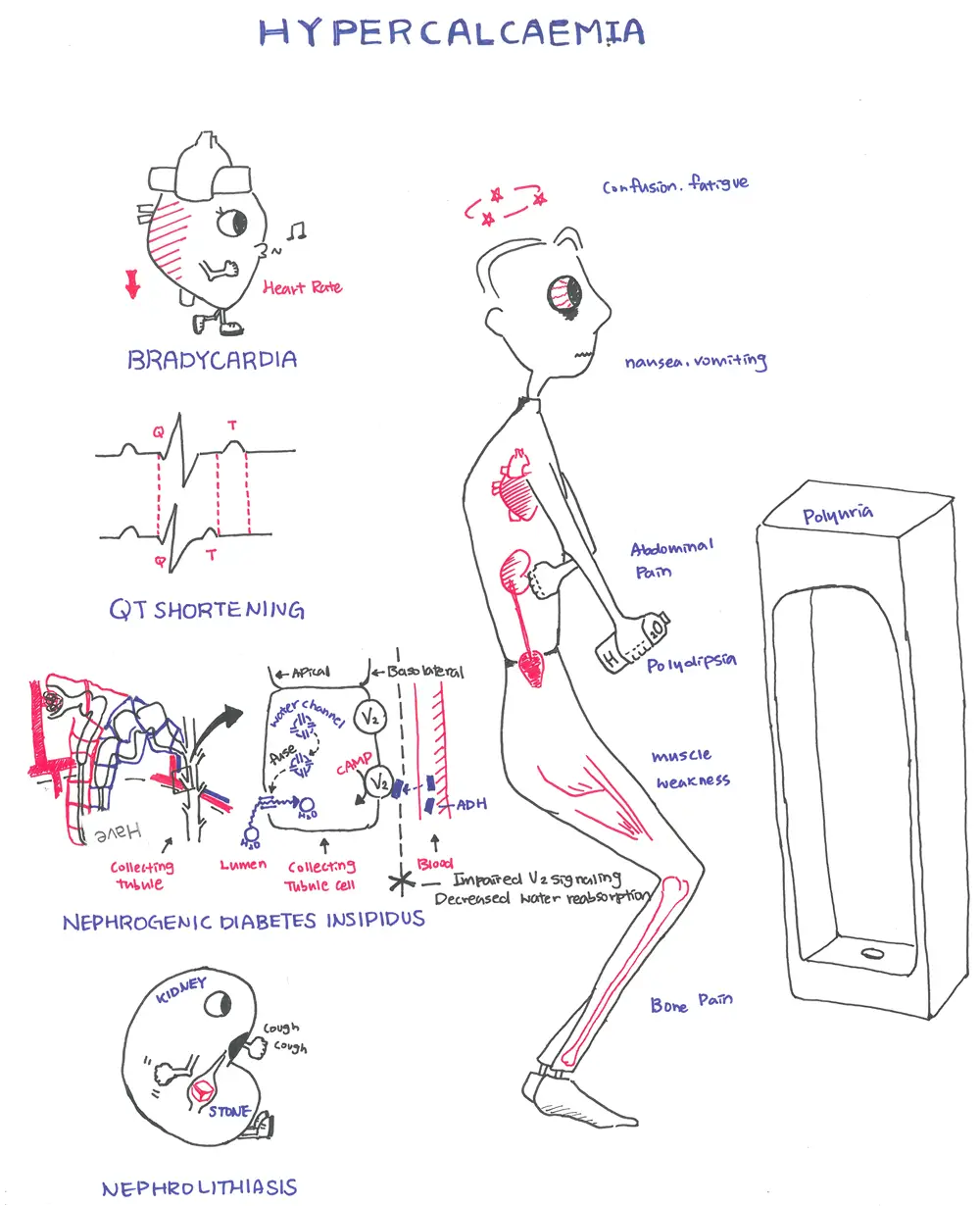
Clinical Presentation
“Bones, stones, thrones groans, moans”
- Stones: nephrolithiasis
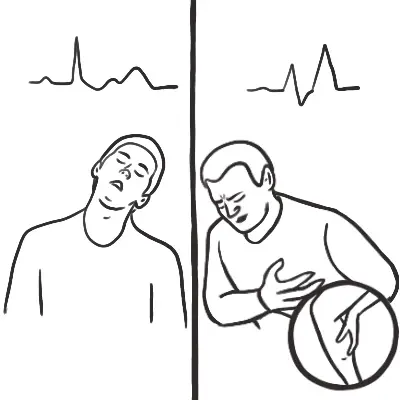
- Bones: bone pain, myalgia, muscle cramps
- Thrones: constipation, polyuria
- Abdominal Groans: abdominal pain
- Psychiatric Moans: anxiety, depression, memory loss, unsteady gait, poor sleep, parasthesia.
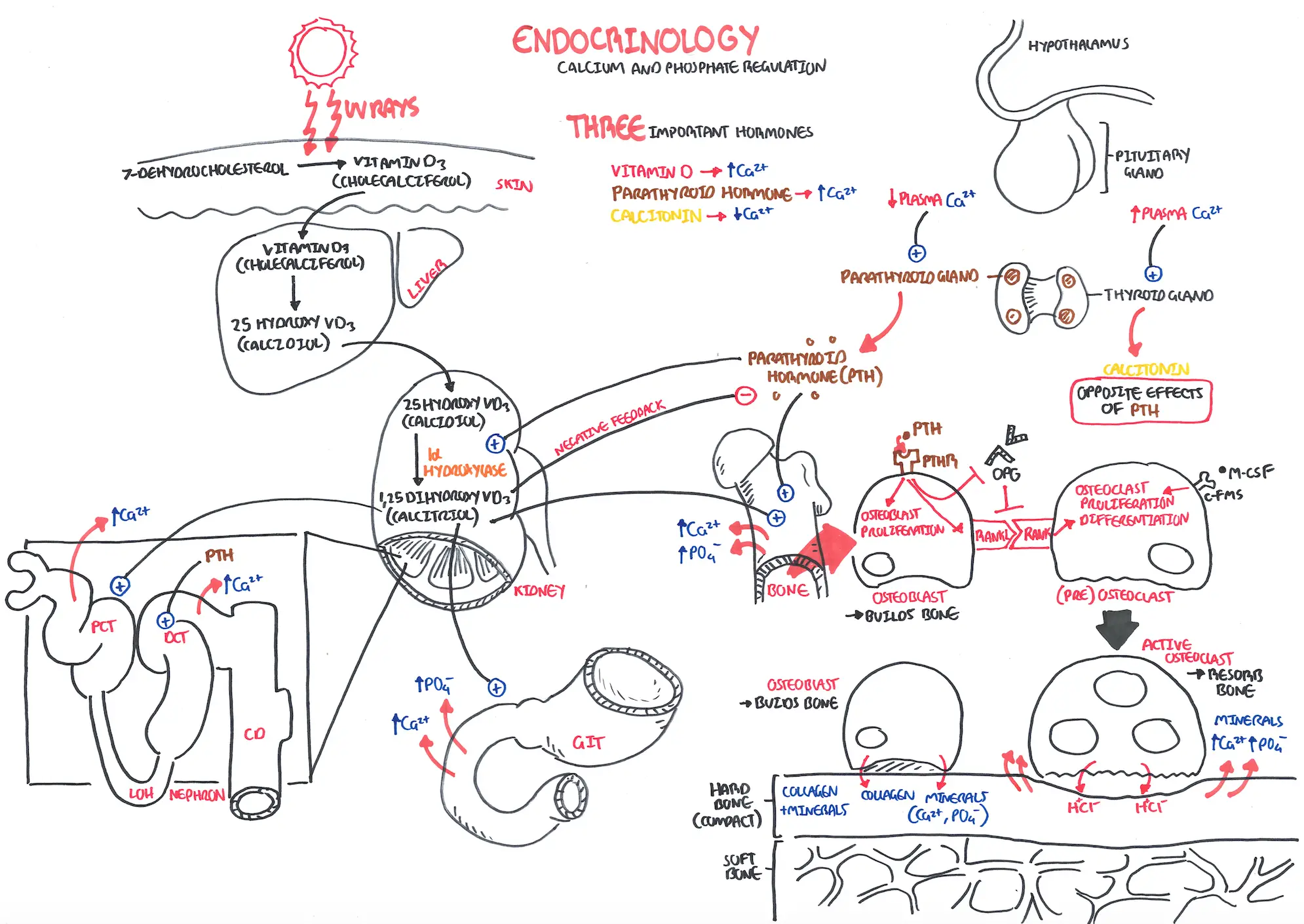
Calcium regulation is primarily controlled by the parathyroid hormone produced by the parathyroid gland. The parathyroid glands are tan-coloured, bean-shaped structures, about the size of a grain of rice. There are 4 parathyroid gland which lie on the posterior surface of the thyroid gland. Parathyroid gland main purpose is to synthesise and secrete parathyroid hormone (PTH). The parathyroid hormone does this in response to blood calcium levels.
- ↓Serum Ca2+ → Stimulates Parathyroidgland → Chief cells secrete PTH → ↑PTH aims to ↑Serum Ca2+
The normal range of serum calcium is 2.25-2.65mmol/L
Calcium is transported in blood bound to albumin. Some travel as free serum calcium.
| Remember Timing and Severity of hypercalcaemia. Sudden = more likely malignancy Chronic = more likely hyperparathyroidism >3.7 really high = malignancy (parathyroid). |
Differential Diagnosis of Hypercalcaemia
- Hyperparathyroidism
- Malignancy
- PTH-like peptide
- Bone metastasis
- Sarcoidosis
- Dehydration and Prolonged immobilisation
- Hyperthyroidism
- Familial hypocalciuric hypercalcaemia
- Drugs
| Remember 90% of hypercalcaemia cases are cause by primary hyperparathyroidism or by malignancy. |
Approach to patient with hypercalcaemia (>2.65mmol/L)
- History
- Examination
- Medication induced hypercalcaemia? → If so, stop medication and observe
- Investigations (DO SERUM PTH FIRST!)
- ↓PTH → Malignancy work up (i.e cancer markers)
- Normal to ↑PTH → 24hour urine calcium level
- ↓24hour urine calcium → Familial Hypocalciuric hypercalcaemia
- ↑24hour urine calcium → Primary or Tertiary Hypercalcaemia
- Other investigation to consider
- PTH
- FBC
- EUC
- Vitamin D
- LFTs
- Thyroid Function test
- Urinary calcium
- Multiple Myeloma screening?
- Management
- Fluids
- Calcitonin
- Bisphosphantes
- Frusemide (to prevent fluid overload)
| Remember 90% of hypercalcaemia is because of malignancy or primary hyperparathyroidism. |
Diagnosis
The diagnosis of hypercalcaemia is made when the corrected serum calcium concentration is 2 standard deviations above the mean of values found in people with normal calcium levels, in at least two samples at least one week apart over a period of three months
| Side note Corrected calcium: ~50% of serum calcium is normally bound to proteins (such as albumin) – therefore leaving only a certain amount bioactive and free. In instances of hypoalbuminemia – there will be more free calcium since it is not bound. |


Discussion