Overview
Hyponatremia is commonly defined as a serum sodium concentration below 130 mmol/L.
- Defined as a serum Na+ <130mmo/L
- It affects 1% of hospital in patients (on call book), 15% (BMJ)
- Most cases require no treatment.
Classification
According to serum ADH levels:
- True volume depletion – gastrointestinal losses (i.e vomiting or diarrhea) or renal losses (i.e thiazides)
- Decreased tissue perfusion (also called effective arterial volume depletion) due to reduced cardiac output in heart failure or to systemic vasodilation in cirrhosis
- A primary (i.e not hypovolemic) increase in ADH release in the syndrome of inappropriate ADH secretion (SIADH)
According to volume status:
- Hypovolemia
- Normovolemia
- Hypervolemia
| Remember Syndrome of Inappropriate ADH (SIADH) is inappropriate secretion of ADH resulting in increased ADH levels in serum and increase ADH activity. |
- Pseudohyponatraemia (arefactual)
- Laboratory analysis technique
- Hyponatraemia with normal serum osmolality
- Hyperlipidaemia, hyperproteinaemia
- Hyponatraemia with increased serum osmolality
- Hyperglycaemia, mannitol, excess urea
- Toxic alcohols (ethanol, methanol, isopropyl alcohol, ethylene glycol)
- Hyponatreamia with high urinary Na+ Indicates inappropriate renal wasting of sodium (rather than retention, which should occur in hyponaturaemia) – Low urine osmolality.
- Hypovolaemia
- Diuretic excess (increase in water and sodium excretion, ADH kicks in > increase water retention).
- Vomiting, NG suction (loss of acid -> increase pH -> kidneys compensate to excrete HCO- with Na+ -> more Na excretion by kidneys)
- Hypoaldosteronism, addisons’ disease, spironolactone (Decrease sodium retention – increase sodium excretion with water).
- Euvolaemia – Due to SIADH
- Malignancy
- CNS disorders – tumours, meningitis, Gullian BS.
- Pulmonary disorders
- GIT
- Drugs – neuroleptics, antidepressants
- Hypervolaemia
- Chronic renal failure (normal urine sodium)
- Hypothyroidism
- Hyponaturaemia with low urinary Na+ indicates appropriate renal conservation of sodium (High Urine osmolality)
- Hypovolaemia
- Diarrhoea (more bicarb excrete in faeces with Na+ kidneys retain Na).
- Sweating, burns, pancreatitis (water and sodium loss – renal system retains more water and sodium – decrease Na excretion from Kidneys. ADH increase more water retention).
- Euvolaemia
- Hypotonic post-op fluids (water moves into RBC)
- Elderly patients with poor diet (tea and toast diet)
- Large volume binge beer drinking
- Hypervolaemia (excess water + sodium in ECF space – reduce Na in blood and urine)
- CCF
- Cirrhosis of liver
- Nephrotic syndrome
- Hypoalbuminaemia
- Hypovolaemia
- Hypovolaemia
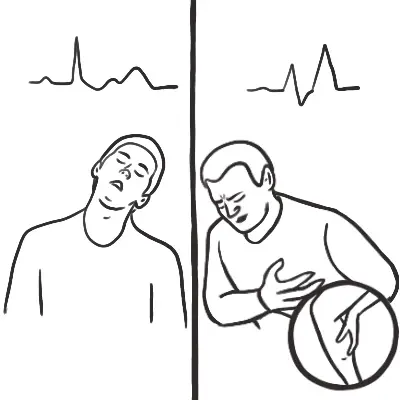
| Remember Increasing sodium to quick can lead to central pontine myelonosis |
Osmotic demyelination syndrome (central pontine myelonosis)
- Rapidly correcting hyponatraemia may produce permanent central nervous system injury, due to osmotic demyelination.
- Patients with chronic hyponatraemia (ie known duration more than 48 hours) are particularly at risk.
- Clinical manifestations typically delayed for 2-6 days.
Symptoms include dysarthria, dysphagia, paraparesis or quadriparesis, behavioural disturbances, movement disorders, seizures, lethargy, confusion, disorientation, obtundation, and coma. Severely affected patients may become “locked in”; they are awake but are unable to move or verbally communicate
Clinical Presentation
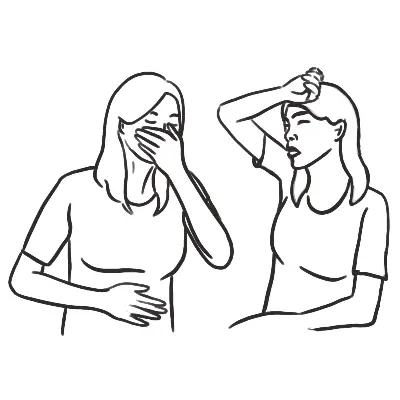
- Mild-moderate
- Lethargy, weakness and ataxia
- Nausea and vomiting
- Headache
- Severe (<120mmols)
- Confusion
- Seizures and coma


Discussion