Basic Calcium Phosphate Disease / Milwaukee Shoulder Syndrome
Basic Calcium Phosphate (BCP) disease is a crystal-associated arthropathy characterized by deposition of BCP crystals in periarticular and intra-articular tissues. A severe clinical presentation of BCP disease is Milwaukee Shoulder Syndrome, which typically affects elderly women, leading to rapid joint destruction, massive rotator cuff tears, and non-inflammatory joint effusion. It often involves the shoulder, but other joints like the hip and knee may be affected.
BCP Crystals: Includes hydroxyapatite, octacalcium phosphate, and tricalcium phosphate; not birefringent and very small.
Milwaukee Shoulder Syndrome (MSS): Rapidly destructive shoulder arthropathy due to BCP crystals, classically in elderly women.
Rotator Cuff Tear Arthropathy: Shoulder joint destruction secondary to long-standing rotator cuff tear, often seen in MSS.
Hydroxyapatite Deposition Disease (HADD): Disease resulting from abnormal deposition of HA crystals in tendons or bursae, leading to pain and inflammation
Calcific tendinitis: Clinical term describing symptomatic HADD, often in the shoulder.
Milwaukee Shoulder Syndrome = Elderly woman + shoulder swelling + rotator cuff tear + non-inflammatory fluid.
Unlike gout/pseudogout, BCP crystals do not cause overt inflammation, but cause chronic degeneration.
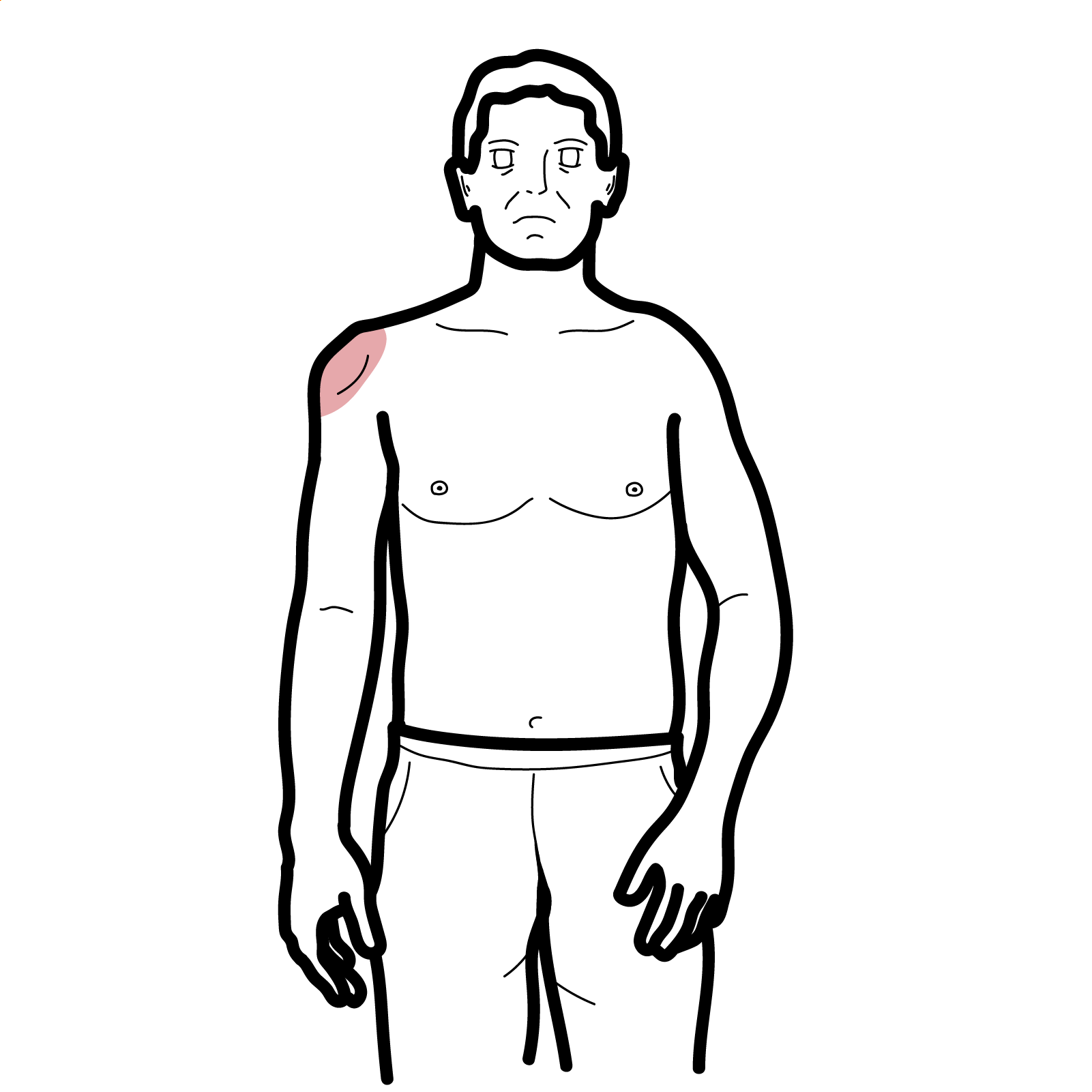
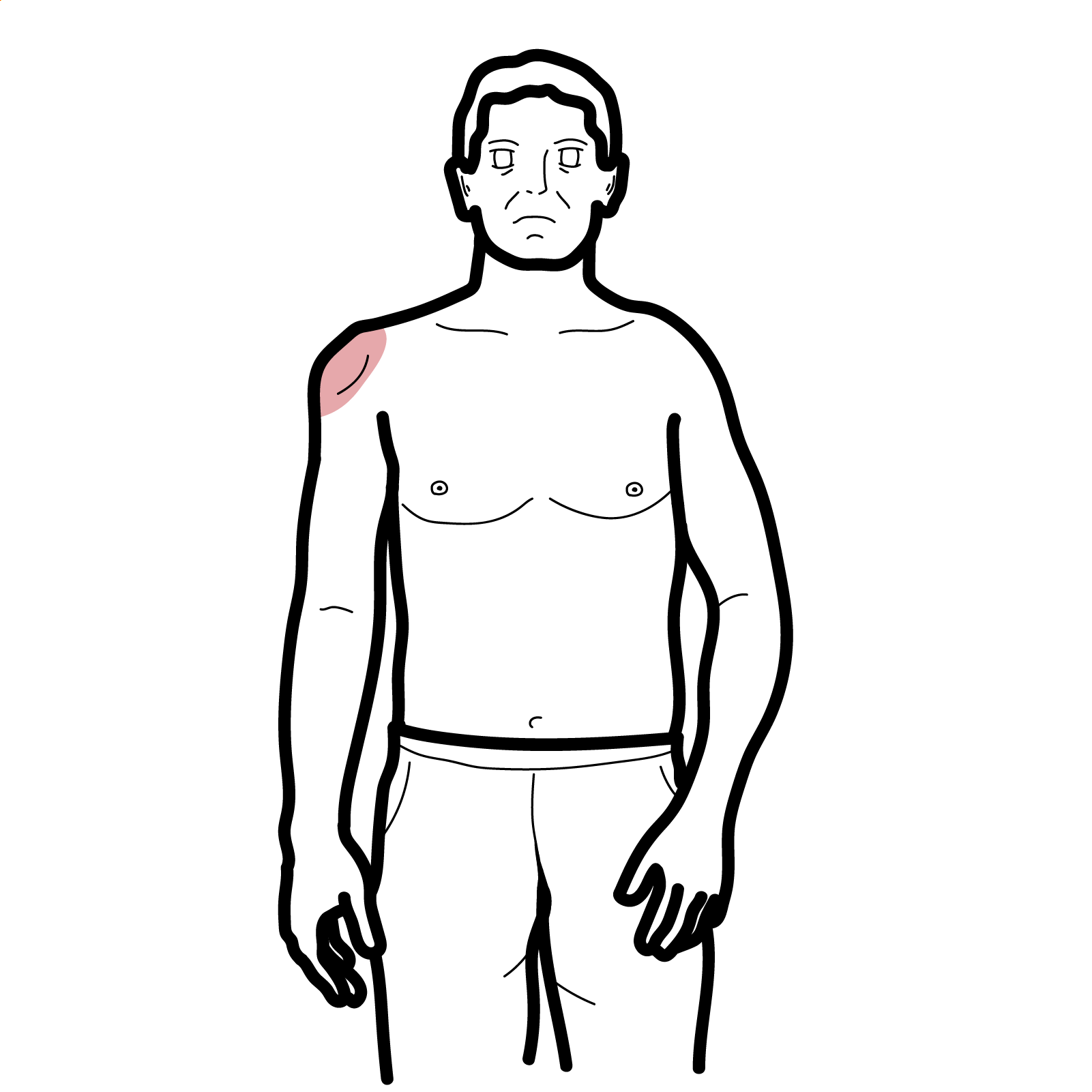
Milwaukee Shoulder Syndrome (classic presentation)
Other features
Triad Milwaukee Shoulder Syndrome: Elderly lady + rotator cuff tear + painless massive effusion
No formal criteria; diagnosis is clinical + imaging + synovial fluid + exclusion of other causes
Imaging
Always aspirate and analyze synovial fluid in an elderly patient with large shoulder effusion before assuming OA or RA.
Fluid is non-inflammatory yet damaging — unlike gout or septic arthritis.
Crystal Arthropathy Clinical Comparison Table
| Feature | Gout | Pseudogout (CPPD) | BCP / Milwaukee Shoulder | HADD (Hydroxyapatite) |
| Typical Age | 30–50 (M > F) | >60 | >70 (F > M) | 30–60 (F > M) |
| Crystal Type & Shape | Monosodium urate, needle | Calcium pyrophosphate, rhomboid | BCP (hydroxyapatite), amorphous | Hydroxyapatite, amorphous |
| Birefringence | Strongly negative | Weakly positive | None | None |
| Common Joint Involved | 1st MTP, midfoot, ankle | Knee, wrist | Shoulder (glenohumeral joint) | Shoulder (supraspinatus tendon) |
| Synovial Fluid WBC | High (2,000–50,000+) | Moderate (2,000–50,000) | Low (<2,000), non-inflammatory | Normal to mildly elevated |
Conservative (mainstay)
Surgical (if severe)

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion