Overview
Chronic widespread pain (CWP) is a nociplastic pain phenotype defined by persistent (≥3 months) pain affecting multiple body regions, with high comorbidity with fatigue, sleep disturbance, mood symptoms and functional impairment. The pooled global prevalence is ~10% (women>men), with higher rates in lower-HDI settings. CWP is recognised in ICD-11 within the chronic primary pain family (fibromyalgia is included).
Major complications include work disability, reduced quality of life and increased all-cause mortality—largely mediated by adverse lifestyle factors—highlighting the need for person-centered, non-drug first care.
Definition
Nociplastic pain: pain from altered nociception without clear tissue damage or somatosensory lesion.
Chronic primary pain (ICD-11): chronic pain as a disease in its own right, with emotional distress/functional disability disproportionate to identifiable pathology; chronic widespread pain is a subgroup (MG30.01) with fibromyalgia listed under it.
Widespread Pain Index (WPI): count of painful sites (0–19) used to quantify pain diffuseness.
“Tender points” are not required for CWP case definition; distribution and duration are.
Classification
Chronic widespread pain is classified under chronic primary pain according to the International Classification of Diseases, 11th Revision (ICD-11). Chronic Primary Pain is pain that persists for ≥3 months and is not better explained by another condition. It is considered a disease in its own right, often associated with emotional distress or functional disability. Examples of chronic primary pain:
- Chronic widespread pain (CWP)
- Fibromyalgia
- Complex regional pain syndrome (CRPS)
- Chronic primary headache
- Chronic primary visceral pain (e.g., irritable bowel syndrome)
- Chronic primary musculoskeletal pain (e.g., non-specific low back pain)
Anatomy & Physiology
- Ascending pathways: peripheral A-delta/C fibres → dorsal horn → spinothalamic/limbic projections → thalamus → S1/S2, insula, anterior cingulate.
- Descending modulation: PAG–RVM circuits modulate dorsal horn via monoamines (5-HT/NA) and endogenous opioids.
- Sleep–pain crosstalk: slow-wave sleep supports descending inhibition; deprivation augments temporal summation.
- Autonomic–HPA axis: sympathetic arousal and cortisol rhythms influence pain thresholds and fatigue.
Changes in sleep and stress biology can shift pain gain as much as structural findings on imaging.
Aetiology and Risk Factors
Aetiology (multifactorial)
- Central sensitisation with impaired descending inhibition (nociplastic mechanism).
- Neuroimmune/glial activation within pain networks (insular/ACC circuits).
- Multisite pain loading and prior regional pains predispose to generalisation.
- Biopsychosocial drivers: adverse life events, psychological distress, deconditioning.
Risk factors
- Female sex, midlife
- Sleep problems (initiation/maintenance/early awakening/non-restorative sleep)
- Fatigue (independent predictors over 5–18 years)
- Higher baseline number of pain sites
- Low socioeconomic/HDI
- Obesity/inactivity
- Anxiety/depression
Ask first about sleep quality and number of pain sites—both predict onset and persistence.
Pathophysiology
- Predisposition (sex, genetics, early adversity, low SES) → lower thresholds for central pain amplification.
- Triggers (regional pain, injury/stress, sleep disruption) → increased peripheral input and stress reactivity.
- CNS changes: augmented temporal summation, reduced conditioned pain modulation, altered insula/ACC connectivity and neurotransmitters (↓NA/5-HT, ↑glutamate); glial activation sustains hyperexcitability.
- Systemic correlates: autonomic dysregulation and sleep fragmentation perpetuate pain and fatigue → generalisation from regional to widespread pain.
Objective inflammation or neuropathic deficits point to secondary causes—reframe diagnosis if present.
Clinical Manifestations
- Pain: chronic (≥3 months), widespread or multisite; migratory/variable intensity; hyperalgesia/allodynia to light pressure.
- Somatic symptoms: fatigue, morning stiffness, headaches/migraine, paresthesias, irritable bowel/bladder, TMJ pain.
- Sleep/cognitive: non-restorative sleep, insomnia, “brain-fog” (attention/processing speed).
- Mood/autonomic: anxiety/depression common; orthostatic intolerance, palpitations, thermodysregulation.
- Clinical Examination
- Normal joint exam
- Normal neurological exam
- Diffuse tenderness to ~4 kg pressure

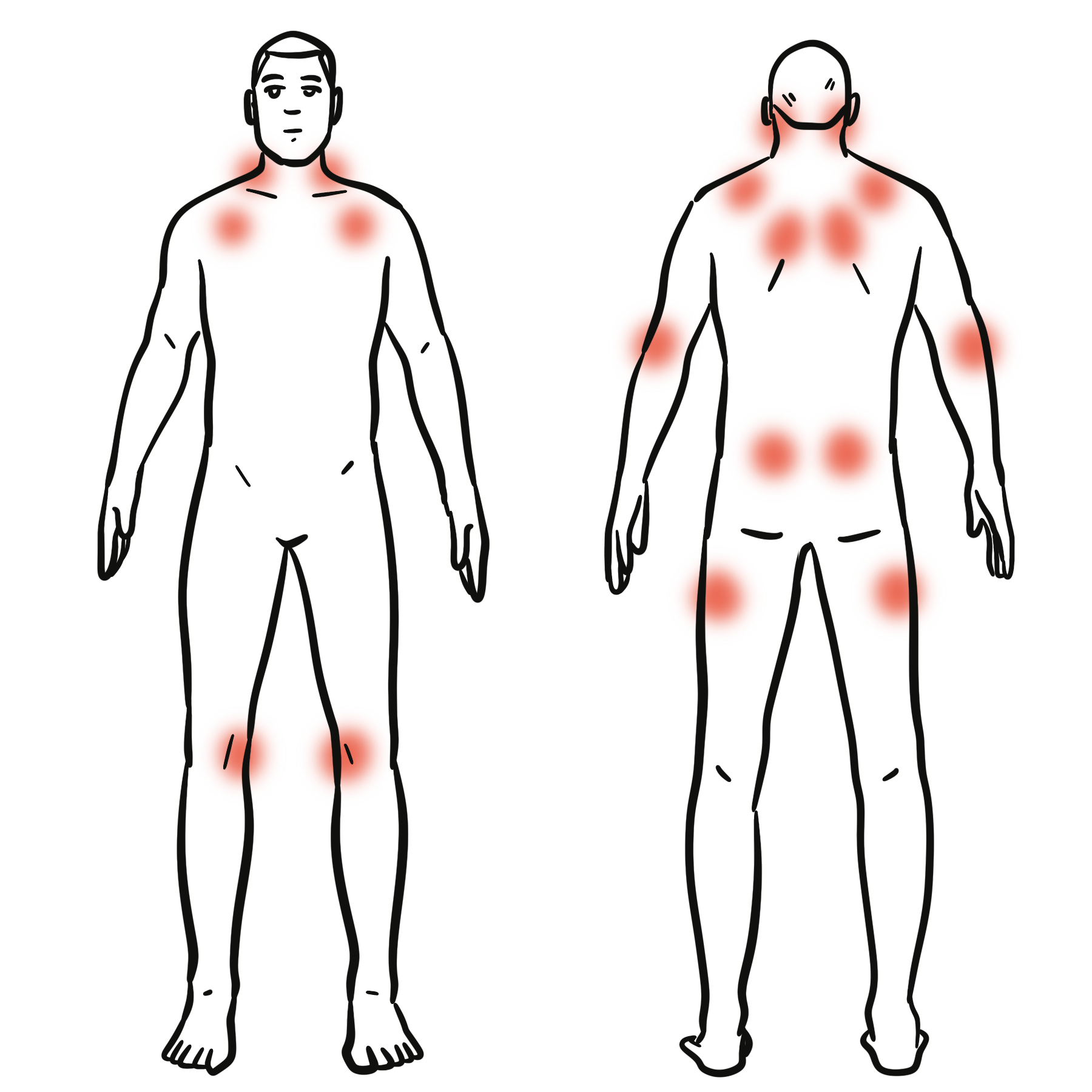
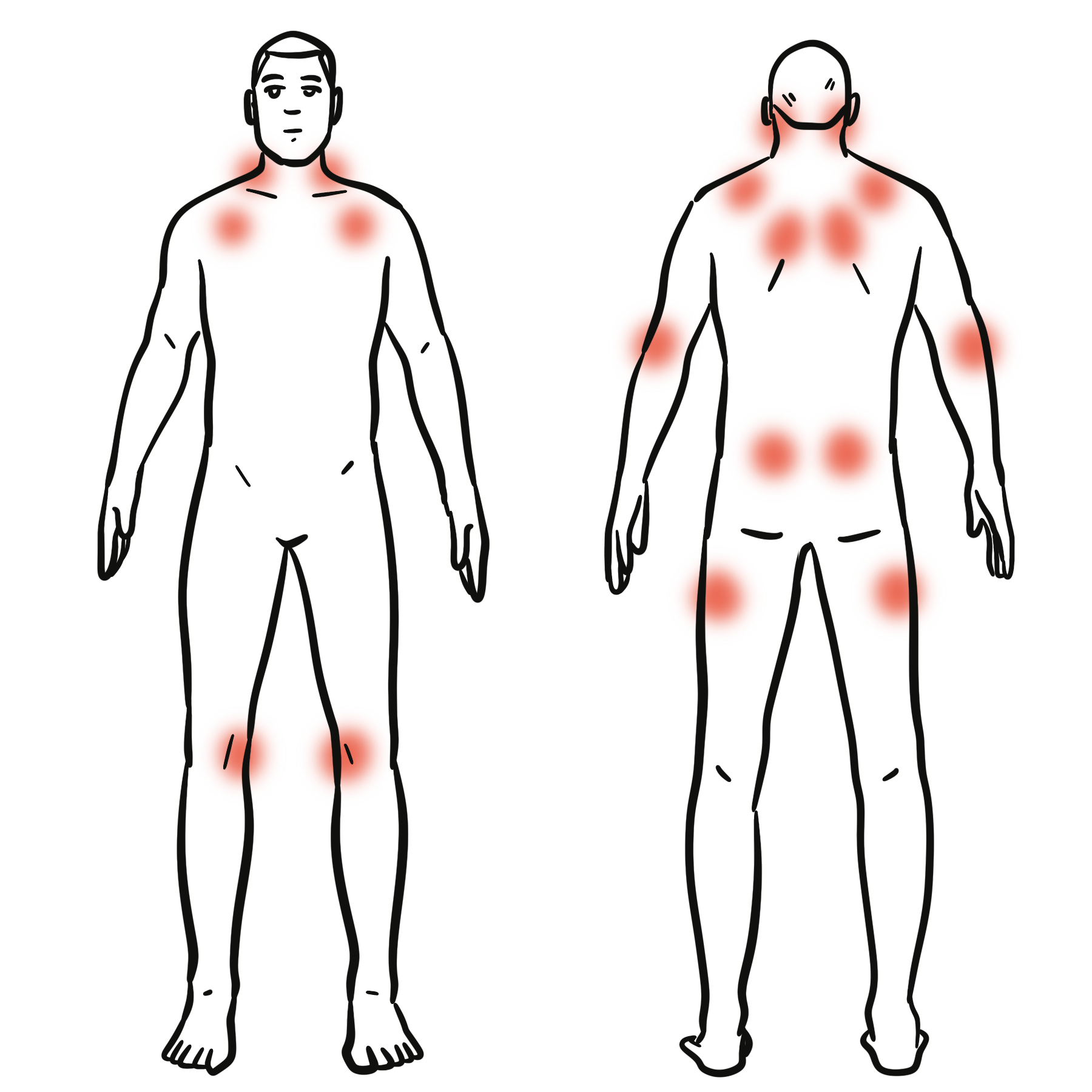
This image series is only available to members
Triad: Widespread pain + Fatigue + Non-restorative sleep.
Severity tracks with polysymptomatic distress (WPI + symptom burden), not imaging findings.
Diagnosis
2019 WP (ACTTION-APS) Case Definition for CWP
To meet the case definition for Chronic Widespread Pain (CWP):
- Duration:
- Pain must be present for ≥3 months.
- Distribution:
- Pain must be present in at least 4 of 5 body regions, which are:
- Left upper region (includes shoulder, arm)
- Right upper region
- Left lower region (includes hip, leg)
- Right lower region
- Axial region (neck, back, chest, abdomen)
- Exclusion of jaw, chest, and abdominal pain as regions:
- While axial pain is required, pain solely in the chest, jaw, or abdomen does not count toward the 4-region criterion.
- Widespread pain must not be explainable by another condition.
Investigations (rule-out/minimise over-testing): FBC, ESR/CRP, TSH, CMP ± CK; screen for OSA when indicated; B12/ferritin if fatigue; autoimmune serology only if clinical suspicion (e.g., synovitis/rashes). NICE encourages person-centred assessment and avoids indiscriminate testing
Differential Diagnosis
- Fibromyalgia (meets ACR 2016 FM criteria with higher symptom burden, but phenotypes overlap).
- Inflammatory rheumatic disease (objective synovitis, raised CRP/ESR, erosions).
- Hypothyroidism (TSH↑, clinical features).
- Myopathies (objective weakness, CK↑).
- Small fibre neuropathy (length-dependent burning, reduced IENFD).
- Polymyalgia rheumatica (older age, shoulder/hip girdle stiffness, CRP/ESR↑).
When patient-reported disease activity is high but CRP/ESR and exam are silent, consider coexisting CWP amplifying symptoms.
Treatment
- General measures
- Medications (for chronic primary pain)
- Consider antidepressants (e.g., amitriptyline, duloxetine, fluoxetine, paroxetine, sertraline, citalopram) after shared decision-making; review regularly for benefit–harm.
- NSAIDs
- Do not initiate opioids, benzodiazepines, antiepileptics (except as part of specialist care)
- Address comorbidities
Exercise has the most consistent benefit across pain, function and QoL; start low, go slow to avoid post-exertional flares.
If multiple drugs at moderate doses fail, rebuild the non-pharmacologic base (sleep–activity–psychology) rather than stacking medications.
Complications and Prognosis
Complications
- Functional limitation, reduced QoL and work participation; high healthcare use/polypharmacy; excess mortality relative to non-CWP peers—attenuated by addressing lifestyle risks (physical inactivity, smoking, diet, obesity).
Prognosis
Fluctuating but modifiable course; many improve with multicomponent care; poorer prognosis with high symptom burden, severe sleep disturbance, persistent psychosocial stressors and multiple pain sites.
Tackling lifestyle mediators (activity, weight, smoking) is part of mortality-risk reduction in CWP.
References
- Wolfe F, Butler SH, Fitzcharles MA, et al. Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria. Scand J Pain. 2020;20(1):77-86. (De Gruyter Brill)
- Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for ICD-11. Pain. 2019;160(1):19-27. (The Erythromelalgia Association)
- NICE Guideline NG193. Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain. 2021. (NICE)
- Andrews P, Steultjens M, Riskowski J. Chronic widespread pain prevalence in the general population: a systematic review. Eur J Pain. 2018;22(1):5-18. (Wiley Online Library)
- Aili K, Andersson M, Bremander A, et al. Sleep problems and fatigue as predictors for the onset of chronic widespread pain over a 5- and 18-year perspective. BMC Musculoskelet Disord. 2018;19:390. (BioMed Central)
- Macfarlane GJ, Barnish MS, Jones GT. Persons with chronic widespread pain experience excess mortality: longitudinal results from UK Biobank and meta-analysis. Ann Rheum Dis. 2017;76(11):1815-1822. (ard.bmj.com, aura.abdn.ac.uk)
- Butler S, Landmark T, Glette M, Borchgrevink P, Woodhouse A. Chronic widespread pain – the need for a standard definition. Pain. 2016;157(3):541-543. (De Gruyter Brill)

Discussion