Overview
CRPS is a disproportionate, regional pain syndrome of a limb that typically follows injury or surgery and features sensory, vasomotor, sudomotor/oedema, and motor/trophic changes. The prevalence after limb fracture/surgery varies widely (≈1–7% overall, higher in some distal radius cohorts) and early recognition with rehabilitation improves outcome. Important risk factors include fracture (especially wrist/ankle), immobilisation, high pain intensity, female sex and psychological distress; major complications are chronic disability, dystonia/contracture, osteoporosis, and reduced return-to-work [2,14,10,6].
Definition
CRPS: persistent regional pain disproportionate to any inciting event, with clinical signs/symptoms in ≥2 of 4 domains (sensory, vasomotor, sudomotor/oedema, motor/trophic) after exclusion of better diagnoses (Budapest criteria).
CRPS I vs II: type I without identifiable nerve injury; type II (causalgia) with definable nerve lesion.
“Warm” vs “Cold” CRPS: phenotypes reflecting vasodilated (erythematous, warm; more inflammatory early) vs vasoconstricted (blue/cold; often later/chronic) presentations.
Allodynia/hyperalgesia: pain to light touch/pinprick greater than expected; central sensitisation hallmark.
CRPS is a clinical diagnosis; imaging/labs are supportive or to exclude mimics, not required for diagnosis.
If features are purely neuropathic without autonomic/motor signs, consider isolated peripheral nerve injury rather than CRPS.
Anatomy & Physiology
- Pain pathways: peripheral nociceptors → dorsal horn → spinothalamic/limbic circuits (insula/ACC); descending modulation via PAG–RVM (5-HT/NA, endogenous opioids).
- Autonomic control: sympathetic vasomotor and sudomotor fibres regulate skin temperature, colour and sweating.
- Neuro-immune interface: neuropeptides (substance P, CGRP) and cytokines modulate vasodilation/oedema; glial activation sustains central sensitisation.
Sleep and stress axes (ANS/HPA) amplify nociception—screen for insomnia/anxiety early.
Aetiology and Risk Factors
Aetiology
- Multimechanistic: neurogenic inflammation (neuropeptides/cytokines), small-fibre dysfunction, autoantibody phenomena (subset), central sensitisation, and maladaptive cortical re-organisation [2,0].
- Precipitating events: fracture, surgery, sprain, crush injury, rarely without major trauma; higher with distal radius/ankle injuries and prolonged immobilisation [2,10].
Risk factors
- Female sex, middle age
- High early pain/cast tightness
- Immobilisation
- Anxiety/depression
- Smoking
- Prior CRPS
- Nerve injury (CRPS II)
Prevention—early mobilisation, good fracture care, patient education; vitamin C 500 mg/d for 6 weeks after wrist fracture may reduce risk (evidence mixed) [3,19].
Pathophysiology
- Inciting injury/surgery → intense nociceptive input + local neurogenic inflammation → vasomotor/sudomotor changes and oedema.
- Peripheral/central sensitisation → allodynia/hyperalgesia; cortical sensorimotor changes maintain pain and neglect-like phenomena.
- Autonomic dysregulation → “warm” (vasodilated) early phenotype; with time some progress to “cold” (vasoconstricted) phenotype with trophic change and dystonia [15].
- Disuse from pain/fear → stiffness, weakness, contractures; bone demineralisation.
Not all patients follow the same path—phenotype (warm vs cold) can guide therapy emphasis (anti-inflammatory/activation vs aggressive desensitisation/contracture prevention) [15,2].
Clinical Manifestations
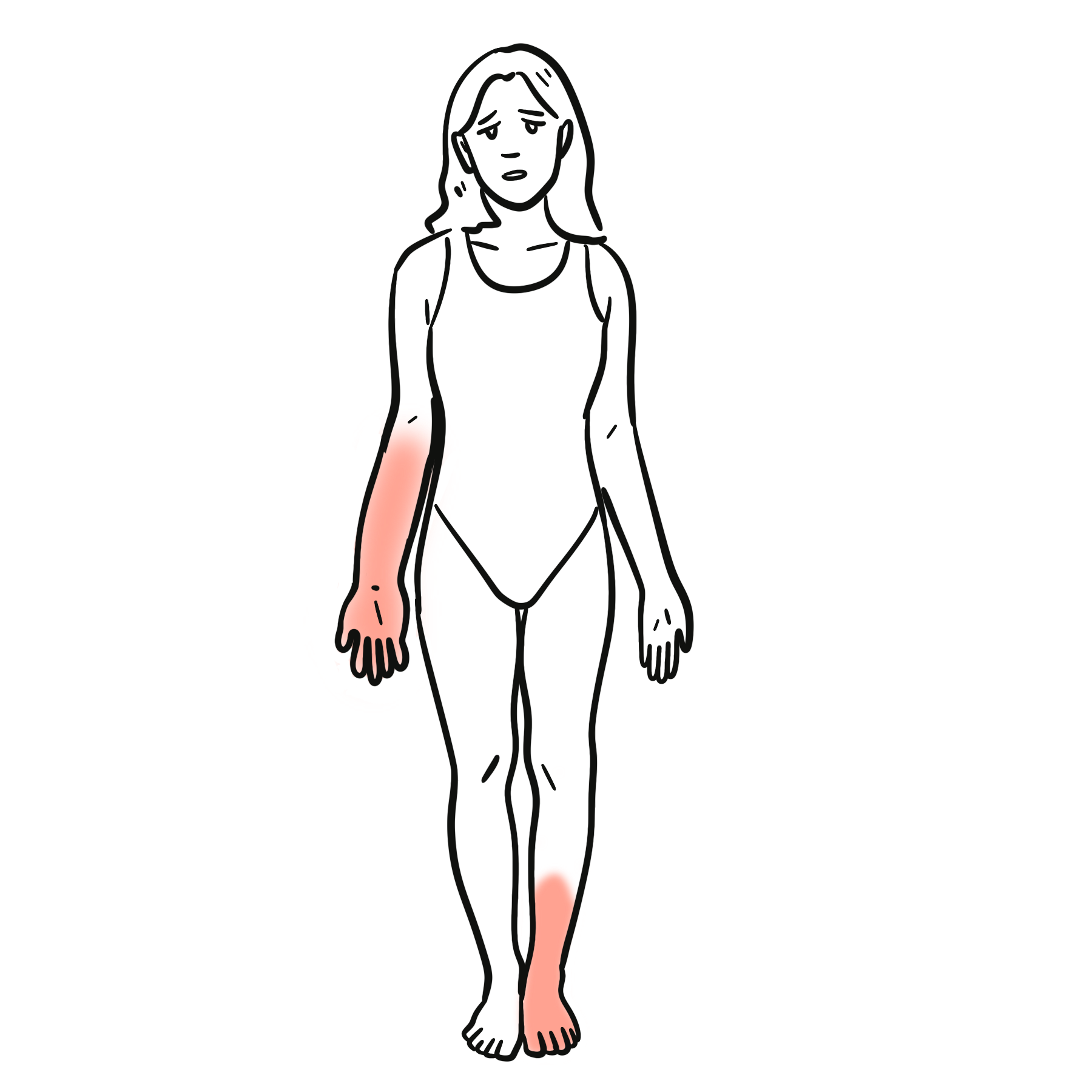
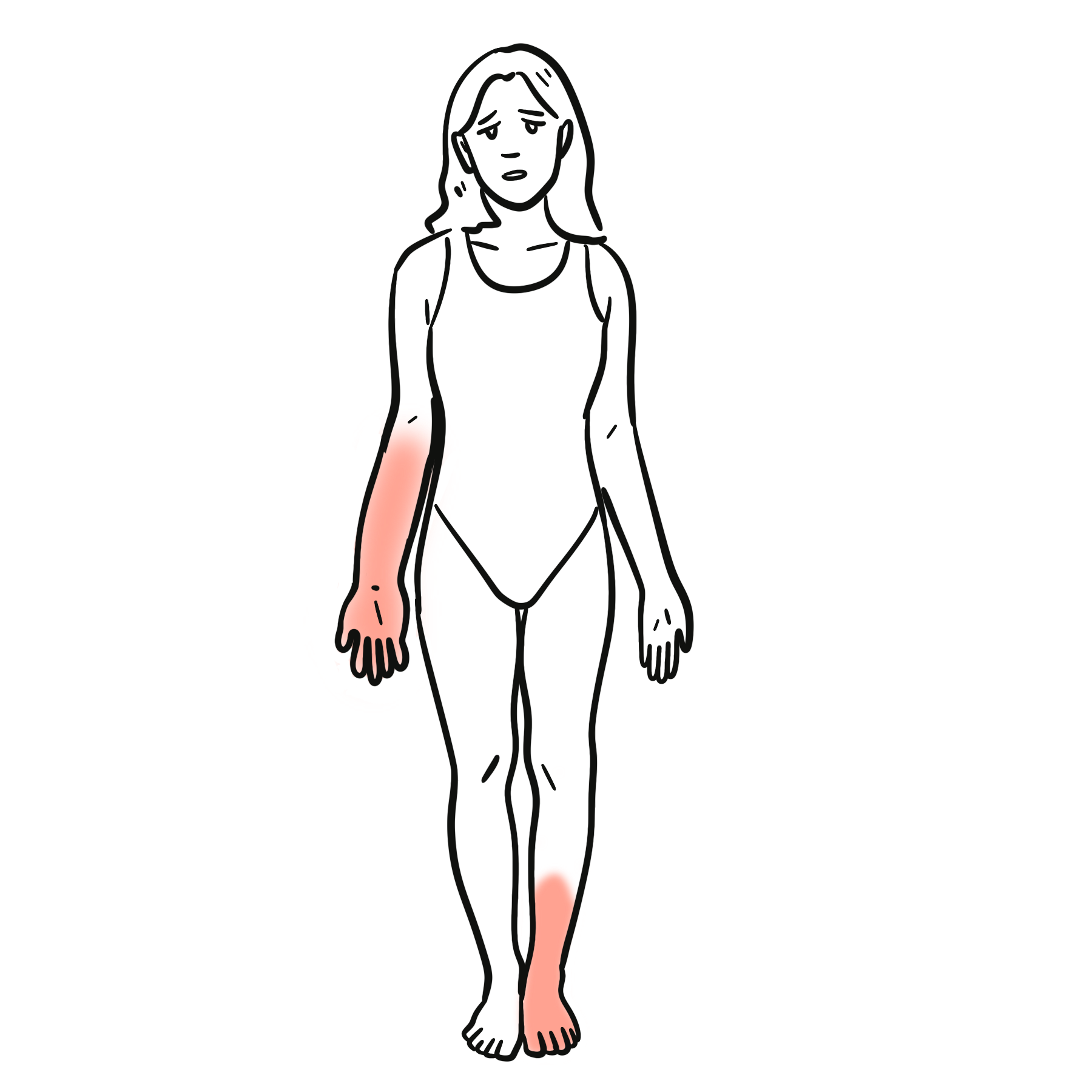
- Pain: regional, continuous, disproportionate to injury; burning/deep ache; mechanical/thermal allodynia and hyperalgesia.
- Vasomotor: temperature or colour asymmetry (warm/red or cold/blue).
- Sudomotor/oedema: swelling, sweating asymmetry.
- Motor/trophic: weakness, tremor/dystonia, decreased ROM, nail/hair/skin changes; neglect-like symptoms or motor imagery difficulty.
Triad (practical): Disproportionate regional pain + Autonomic/trophic change + Movement limitation.
Diagnosis
Budapest clinical criteria
- Ongoing pain that is disproportionate to any inciting event.
- Presence of at least one symptom in three of the following four categories:
- Sensory: hyperesthesia or allodynia
- Vasomotor: temperature asymmetry or skin colour changes/asymmetry
- Sudomotor/oedema: oedema, sweating changes or sweating asymmetry
- Motor/trophic: decreased range of motion, motor dysfunction (e.g., weakness, tremor) or trophic changes (e.g., altered hair, nail, or skin)
- At least one clinical sign in two or more of the same categories at the time of assessment:
- Sensory: evidence of hyperalgesia or allodynia
- Vasomotor: temperature or skin colour asymmetry
- Sudomotor/oedema: oedema or sweating differences
- Motor/trophic: observable motor dysfunction or trophic changes
- No other diagnosis better explains the signs and symptoms.
Other Investigations (support/exclude)
- Plain x-ray for patchy osteopenia (late)
- MRI for marrow oedema/soft-tissue swelling
- 3-phase bone scan not required and inconsistent
- Thermography
Diagnosis is clinical; do not delay rehabilitation while “waiting for scans”.
Differential Diagnosis
- Cellulitis (fever/leukocytosis, warmth without allodynia)
- DVT (risk factors, duplex positive)
- Compartment syndrome (pain out of proportion + tense compartments)
- Neuropathic pain from specific nerve lesion (topographic distribution)
- Inflammatory arthritis (synovitis, raised CRP/ESR)
- Erythromelalgia (heat/redness without trophic/motor changes).
If a clear single-nerve deficit is present, consider CRPS II or focal neuropathy and image/EMG accordingly.
Classification
Complex regional pain syndrome is classified under chronic primary pain according to the International Classification of Diseases, 11th Revision (ICD-11). Chronic Primary Pain is pain that persists for ≥3 months and is not better explained by another condition. It is considered a disease in its own right, often associated with emotional distress or functional disability. Examples of chronic primary pain:
- Chronic widespread pain (CWP)
- Fibromyalgia
- Complex regional pain syndrome (CRPS)
- Chronic primary headache
- Chronic primary visceral pain (e.g., irritable bowel syndrome)
- Chronic primary musculoskeletal pain (e.g., non-specific low back pain)
Complex Regional pain syndrome classification
- By nerve injury: CRPS I (no identifiable nerve lesion) vs CRPS II (definable nerve injury)
- By temperature phenotype: Warm CRPS (vasodilated, often early) vs Cold CRPS (vasoconstricted, often chronic)
- By course: acute/early (<3–6 mo) vs persistent/chronic.
- Paediatric vs adult CRPS (management emphasis differs but Budapest criteria apply)
Treatment
- Foundations
- Education (biopsychosocial model)
- Early limb use and functional restoration
- Desensitisation
- Graded motor imagery (GMI)/mirror therapy
- Structured physiotherapy/occupational therapy with pacing and flare plans
- Analgesic/neuropathic agents (individualised): short course oral corticosteroids early may help pain/oedema; bisphosphonates (e.g., neridronate IV or IM) reduce pain in CRPS-I (moderate evidence); consider gabapentinoids, TCAs/SNRIs; topical agents for focal allodynia; avoid long-term strong opioids [4,12,20,17].
- Interventional (refractory, specialist)
- Dorsal root ganglion (DRG) stimulation offers higher treatment success than conventional spinal cord stimulation (SCS) at 3–12 months in lower-limb CRPS;
- SCS remains an option
- Consider sympathetic blocks for selected warm/vasomotor-dominant cases
- Ketamine infusions and IV lidocaine only in specialised centres with careful selection [3,1,9].
- Prevention after fracture
- Encourage early mobilisation
- Vitamin C 500 mg daily for 6 weeks after wrist fracture may lower incidence though evidence is mixed
- Paediatric focus
- Intensive physiotherapy + psychology (exposure, CBT
- school reintegration; medications are adjunctive [2].
Remember: Functional restoration is the primary goal; medications and procedures are adjuncts, not substitutes [2,6].
Cold, chronic CRPS with contracture needs aggressive ROM/functional programmes and splinting; monitor for osteoporosis/disuse.
Complications and Prognosis
Complications
- Contractures/dystonia
- Chronic functional limitation
- Disuse osteopenia/osteoporosis
- Depression/anxiety
- Medication harms
- Persistent oedema/skin changes
Prognosis
- Many improve within the first year with early rehab
- A subset progress to chronic cold CRPS with disability
- Poor prognostic factors include delayed diagnosis/treatment, cold phenotype, high early pain, psychological distress, and prolonged immobilisation [2,15]
Early interdisciplinary care and return-to-function planning are the strongest modifiable prognostic lever.
References
- Deer TR, Levy RM, Kramer J, et al. Therapy habituation at 12 months: dorsal root ganglion versus spinal cord stimulation in CRPS. J Pain. 2019;20(5):551–561. (Jpain)
- Royal College of Physicians. Complex regional pain syndrome in adults (2nd ed.). London: RCP; 2018. (rcp.ac.uk)
- Harden RN, Bruehl S, Perez RS, et al. Complex Regional Pain Syndrome: Practical Diagnostic and Treatment Guidelines, 5th ed. RSDSA; 2022. (issp-pain.org)
- Varenna M, Adami S, Sinigaglia L, et al. Treatment of CRPS-I with neridronate: randomized placebo-controlled trial. Rheumatology (Oxford). 2013;52(3):534–542. (Oxford Academic)
- Limakatso K, Madden V, Parker R. Graded motor imagery and mirror therapy for CRPS: systematic review. Biomedicines. 2023;11(9):2140. (MDPI)
- Ferraro MC, Cashin AG, Wand BM, et al. Interventions for treating pain and disability in adults with CRPS: overview of systematic reviews. Cochrane Database Syst Rev. 2023;CD009416. (Cochrane)
- IASP. Complex Regional Pain Syndrome Special Interest Group. 2024. (IASP)
- Harden RN, Bruehl S, Perez RS, et al. Validation of the Budapest Criteria for CRPS. Pain. 2010;150(2):268–274. (ScienceDirect, baycrest.echoontario.ca)
- Pain Relief Foundation. Clinical practice guideline review of reviews for CRPS management (2022). (painrelieffoundation.org.uk)
- Kim HS, Jang CY, Kim JH, et al. Incidence and risk factors for CRPS after radius fractures: meta-analysis. Arch Orthop Trauma Surg. 2023;143(11):6639–6652. (SpringerLink)
- Birklein F, Schlereth T. Complex regional pain syndrome—phenotypic characteristics and mechanisms. Nat Rev Neurol. 2018;14(9):607–617. (Nature)
- Varenna M, Zucchi F, Ghiringhelli D, et al. Intramuscular neridronate in CRPS-I: randomized double-blind trial. Pain Med. 2021;22(10):2349–2359. (SAGE Journals, Europe PMC)
- Faculty of Pain Medicine (UK). Criteria for diagnosis of CRPS (Budapest). 2021. (Faculty of Pain Medicine)
- Macfarlane GJ et al. CRPS epidemiology (summary). BMJ. 2015;351:h2730. (BMJ)
- Bruehl S, et al. Evidence for warm and cold CRPS subtypes. Pain. 2016;157(8):1674–1683. (Lippincott Journals)
- Ferraro et al. Cochrane—physiotherapy for CRPS (background). Cochrane Database Syst Rev. 2015;CD010853. (Cochrane Library)
- Cochrane overview and RSDSA guideline sections on steroids/ketamine (2022–2023). (Cochrane, issp-pain.org)
- BSSH link to RCP guideline summary. 2018. (bssh.ac.uk)
- Song K, et al. Vitamin C for preventing/treated CRPS: updated evaluation. Front Surg. 2024;11:1473311. (ScienceDirect)

Discussion