Enteropathic Arthritis
Enteropathic arthritis is a subtype of spondyloarthropathy associated with inflammatory bowel disease (IBD), particularly Crohn’s disease and ulcerative colitis. It affects up to 20% of IBD patients, with a variable presentation involving axial and/or peripheral joints. The arthritis may run parallel to intestinal disease activity or occur independently, often with enthesitis or dactylitis. It has no gender predilection and usually presents in young adults (20–40 years).
Enteropathic arthritis: Inflammatory arthritis associated with IBD (Crohn’s or UC)
Spondyloarthropathy: Group of inflammatory rheumatic diseases with overlapping features including axial arthritis, enthesitis, and HLA-B27 association
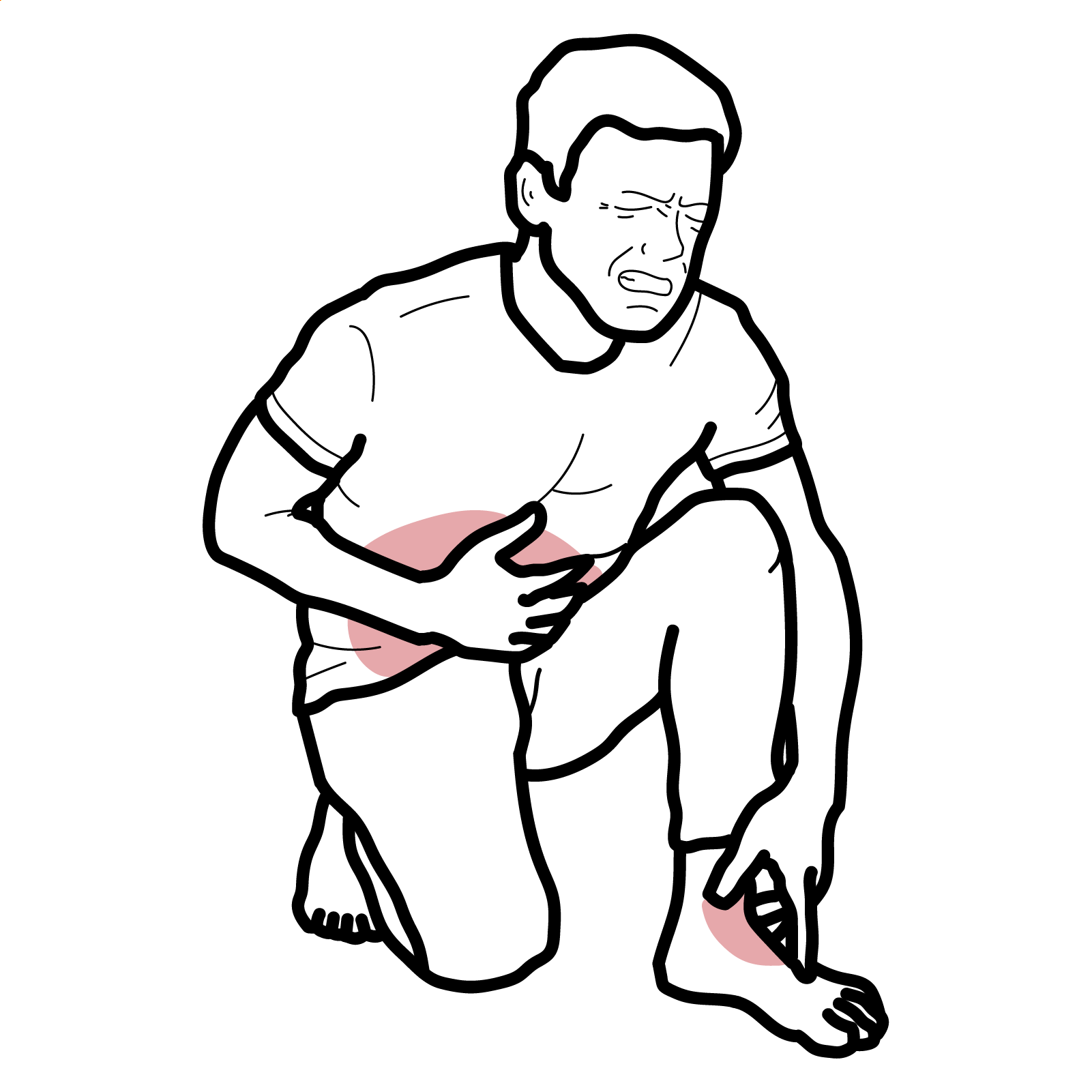
Enthesitis: Inflammation at tendon/ligament attachment sites
Dactylitis: Diffuse swelling of entire digits (“sausage digit”)
• Loss of intestinal barrier integrity → translocation of microbial antigens
• Activation of innate and adaptive immunity (Th17, IL-23 axis)
• Immune-mediated joint inflammation (molecular mimicry, shared antigens)
• In axial disease, chronic enthesitis may lead to new bone formation and ankylosis
Parallel flares of gut and joint symptoms may suggest a shared inflammatory driver.
Type 1 arthritis flares with IBD; Type 2 is persistent and more symmetric.
No formal diagnostic criteria specific to enteropathic arthritis; typically classified under spondyloarthritis using:
Investigations
Differential Diagnoses:
| Condition | Clinical features |
| Reactive arthritis | Recent GI/GU infection, resolves in 6 months |
| Psoriatic arthritis | Skin and nail psoriasis, dactylitis, family history |
| Rheumatoid arthritis | Symmetric polyarthritis, positive RF/anti-CCP |
| Septic arthritis | Acute monoarthritis, fever, positive culture |
Consider enteropathic arthritis in young adults with unexplained arthritis and bowel symptoms.
Non-pharmacological:
• Physiotherapy and joint protection
• Manage IBD with gastroenterologist collaboration
Pharmacological:
• NSAIDs: Use with caution in IBD (can exacerbate bowel symptoms)
• Corticosteroids: Short-term for flares
• Sulfasalazine: Effective in peripheral arthritis
• Methotrexate: Consider for peripheral involvement, especially in Crohn’s
• Anti-TNF agents (infliximab, adalimumab): Effective for both joint and gut inflammation
• IL-12/23 inhibitors (ustekinumab): Used in Crohn’s with joint symptoms
• IL-17 inhibitors (e.g. secukinumab) are not recommended in IBD
Anti-TNFs are the cornerstone for dual control of joint and bowel inflammation.
IL-17 inhibitors (e.g. secukinumab) are not recommended in IBD.
Complications
Poor prognostic factors
– Early-onset polyarthritis
– Persistent IBD activity
– Axial involvement with HLA-B27
– Delay in diagnosis and treatment

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion