Overview
Melanoma accounts for 4 percent of all dermatological cancer. Melanoma has the highest mortality rate of all dermatological cancers, only 14 percent of patients with metastatic melanoma survive for five years. Melanoma is one of the most common cancers in young adults.
| Video: Melanoma Overview |
Anatomy and Physiology
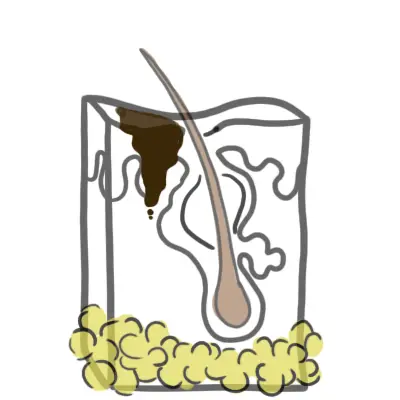
The skin consist of three layers, from superficial to deep:
- Epidermis
- Dermis
- Papillary layer
- Reticular layer
- Hypodermis (some don’t classify it as skin)
The epidermal layer are made up mainly of keratinocytes, which are squamous epithelial cells high in keratin (protein). Other cells residing in the epidermis include:
- Melanocytes – produce melanin
- Langerhan cells – immune cell, basically a dendritic cell of the skin
- Merkel Cells – tactile cells for sensation
Melanocytes are mature melanin-forming cells found in many parts of the body (eye, ear, hair, heart, bone), but especially in the skin. Through a process called melanogenesis, these cells produce melanin, which is a pigment found in the skin, eye and hair. Vitamin D and UV light stimulate melanocytes to produce melanin.
| Watch Dermatology Introduction |
Pathophysiology
- Melanoma arises from melanocytes
- Genetics and environmental factors play a role in the pathogenesis
- A proportion of melanoma arise from pre existing naevi
Pathophysiology
Mutated BRAF and NRAS genes are most common in superficial spreading and nodular melanoma.
Pathology
Different types of Melanoma
- Superficial spreading (most common)
- Nodular (most dangerous)
- Lentigo maligna
- Acral lentiginous
| Pathological Differences between Benign and Malignant tumours | |
| Malignant | Benign |
| Invasive | Non-Invasive |
| Poorly differentiated | Well Differentiated |
| High mitotic rate | Normal mitotic rate |
| Non-capsulated | Capsulated |
| Usually large growth | Usually small growth |
| Not well circumscribed | Well circumscribed |
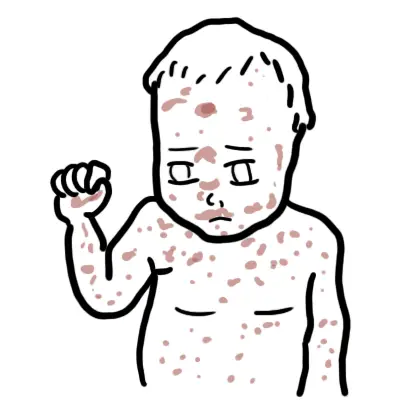
Clinical Manifestation
- Atypical naevi
- Ulceration and bleeding
- Constitutional symptoms
Examination – ABCDE
- A – asymmetry
- B – borders (irregular and/or distinct)
- C – colour (varied)
- D – Diameter (increasing or >6mm)
- E – Elevation and Evolution (most important as in changing rapidly/growing)
| Remember Blanching. Press down on the lesion for ~3 seconds. Release if pale and refills there is a vascularity involved. |
Diagnosis
- Examination ABCDE
- If Melanoma suspected perform a skin biopsy
- Breslow’s thickness can be used to stage Melanoma and establish prognosis
Diagnosis
- Seborrhoeic keratosis
- Pigmented basal cell carcinoma
- Actinic keratosis
- Benign melanocytic naevi
- Spitz naevus
- Haemangioma
| Think Squamous cell carcinoma is not a good differential because it is not pigmented. |
Investigations
- Dermatoscope
- Skin Biopsy
- Chest X-ray for metastasis
| Remember 1.4cm depth is dangerous. |
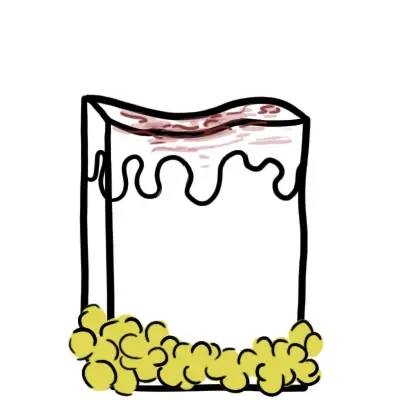
Staging
| Clark’s Staging – Important histologically | |
| Clark’s Level | Histological characteristic |
| I | Confined to the epidermis “in situ” |
| II | Invasion of the papillary dermis |
| III | Filling of the papillary dermis |
| IV | Invasion of the reticular dermis |
| V | Invasion of the deep, subcutaneous tissue |
| Breslow’s Staging – Important Prognostically | |
| Breslow’s Thickness | Depth of tumour invasion |
| I | ≤0.75mm |
| II | 0.75-1.5mm |
| III | 1.51-2.25mm |
| IV | 2.26-3.0mm |
| V | >3.0mm |
Treatment
- Surgical excision
- Topical Imiquimod
- Surgical excision +/- sentinel lymph node biopsy
Complications and Prognosis
Complication
Metastasis
Treatment adverse effects
- Chemotherapy
- Radiotherapy
- Immunotherapy (causes flu-like symptoms)
Prognosis The most important prognostic indicators are Breslow’s depth of the tumour and lymph node status.
- Stage 0 (in-situ melanoma): >98%
- Stage I (Breslow’s depth <1 mm and no nodal or metastatic disease): 90% to 95%
- Stage II (localised disease, intermediate to thick depth): 45% to 78% (78% for non-ulcerated melanoma of depth 1 to 4 mm; 45% for an ulcerated melanoma >4 mm depth)
- Stage III (nodal metastases): 69% (non-ulcerated melanoma of any depth with a single positive node) to 26% (ulcerated melanoma of any depth with 4 or more positive nodes)
- Stage IV (metastatic): overall prognosis is bleak; 3% to 10% depending on the extent and sites of metastasis.

Discussion