Microscopic Polyangiitis
Microscopic polyangiitis (MPA) is a small-vessel necrotizing vasculitis, commonly associated with myeloperoxidase-ANCA (MPO-ANCA) positivity. It typically presents with glomerulonephritis and pulmonary capillaritis, but does not involve granulomatous inflammation, distinguishing it from GPA.Incidence: ~3–24 cases per million annually; more common in middle-aged adults and slightly more frequent in males. 1
MPO-ANCA (Myeloperoxidase-ANCA): An autoantibody typically associated with MPA, targeting myeloperoxidase in neutrophils and contributing to vessel inflammation.
Pauci-immune glomerulonephritis: A type of rapidly progressive kidney inflammation seen in MPA with little or no immune complex deposition on biopsy.
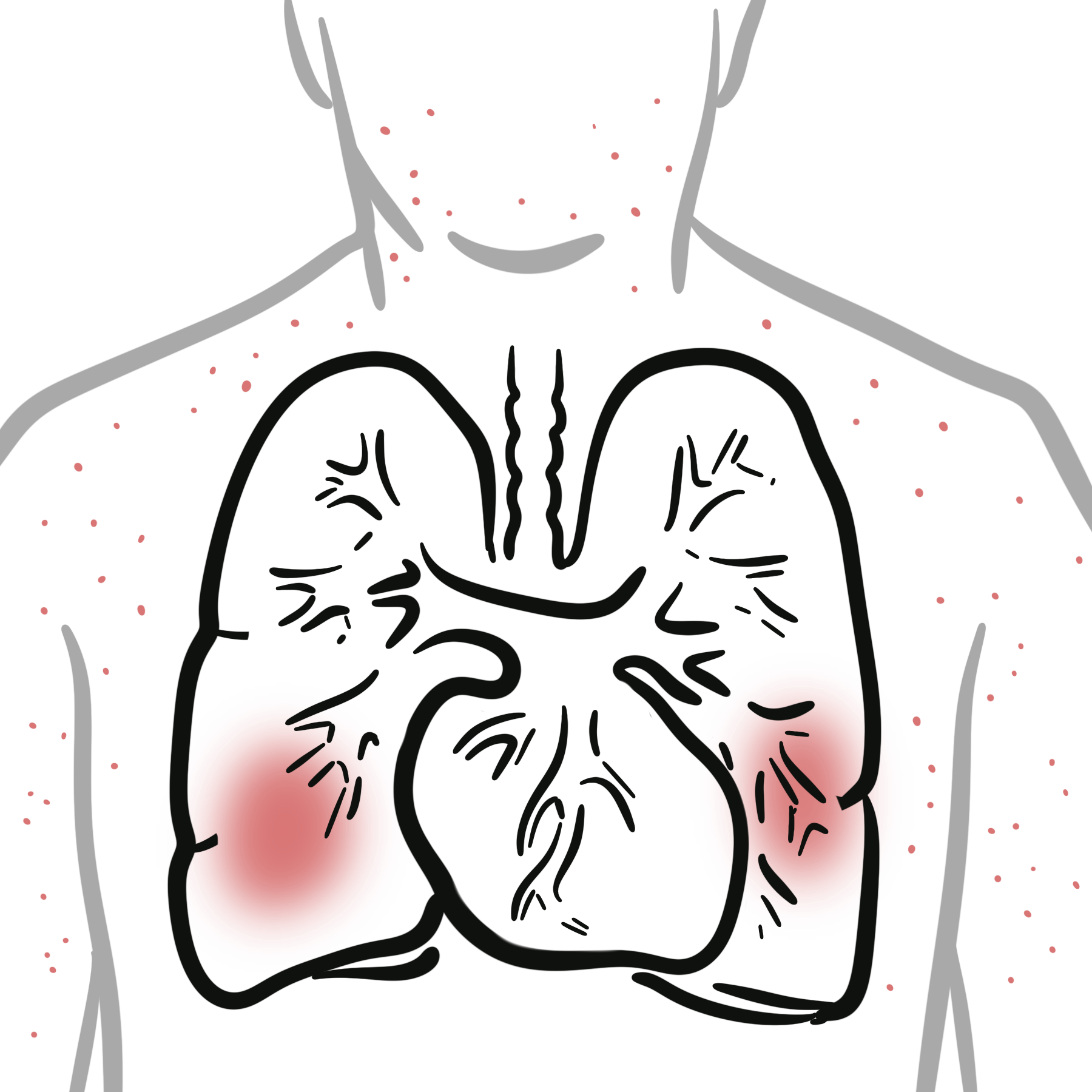
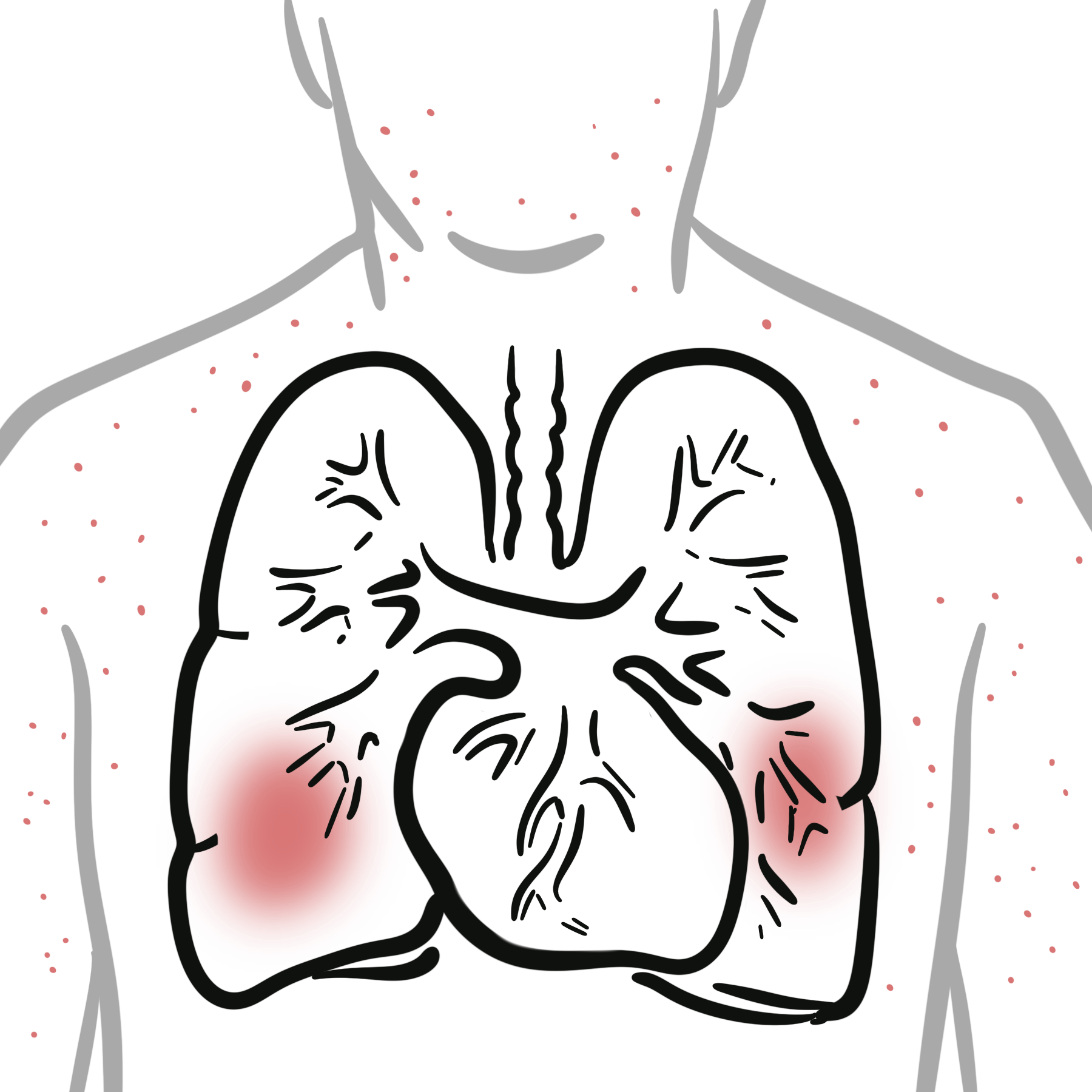
Pulmonary capillaritis: Inflammation of lung capillaries leading to alveolar hemorrhage, a serious respiratory complication of MPA.
Necrotizing vasculitis: Destructive inflammation of small to medium-sized blood vessels without granulomas, characteristic of MPA.
MPA affects small vessels, including capillaries, venules, and arterioles. Involvement often includes:
Pulmonary-renal syndrome in a patient with MPO-ANCA strongly suggests MPA. However GPA and Anti-GBM also involve pulmonary-renal syndrome (typically with other autoantibodies).
Skin: Palpable purpura, ulcers
ENT involvement is uncommon in MPA (minus points) – unlike GPA.
Pulmonary haemorrhage is most common with MPA>GPA>EGPA.
Classification Criteria (2022 ACR/EULAR)
| Entry Requirement: A diagnosis of small- or medium-vessel vasculitis has been made (biopsy), and other mimicking conditions have been excluded. | |||
| Variables | GPA | MPA | EGPA |
| Clinical criteria | |||
| Nasal passage involvement | +3 | −3 | — |
| Cartilaginous involvement | +2 | — | — |
| Conductive or sensorineural hearing loss | +1 | — | — |
| Obstructive airway disease | — | — | +3 |
| Nasal polyp | — | — | +3 |
| Mononeuritis multiplex | — | — | +1 |
| Laboratory criteria | |||
| PR3-ANCA (or C-ANCA) positivity | +5 | −1 | −3 |
| MPO-ANCA (or P-ANCA) positivity | −1 | +6 | — |
| Serum eosinophil ≥1000/µL | −4 | −4 | +5 |
| Hematuria | — | — | −1 |
| Histological criteria | |||
| Granuloma, granulomatous inflammation, or giant cells | +2 | — | — |
| Pauci-immune glomerulonephritis | +1 | +3 | — |
| Extravascular eosinophilic-predominant inflammation | — | — | +2 |
| Radiological criteria | |||
| Pulmonary nodules, mass, or cavitation on chest imaging | +2 | — | — |
| Fibrosis or ILD on chest imaging | — | +3 | — |
| Nasal/paranasal sinusitis or mastoiditis on imaging | +1 | — | +1 |
| Total Score Cut-off for Classification | ≥5 | ≥5 | ≥6 |
MPA is classified under ANCA-associated vasculitides alongside:
Induction (Severe/Relapse)
Induction (Non-severe)
Maintenance
Supportive
Relapse rates are lower in MPA vs GPA.
Pulmonary hemorrhage occurs in ~12 % of patients with MPA but is associated with high mortality (~10–25 %); importantly, up to half may have silent hemorrhage without hemoptysis.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion