Mixed Connective Tissue Disease (MCTD)
MCTD is a systemic autoimmune rheumatic disease characterized by overlapping clinical features of systemic lupus erythematosus (SLE), systemic sclerosis (SSc), polymyositis, with rheumatoid arthritis with high titres of anti-U1 RNP antibodies. It typically affects women aged 20–40 years. Prevalence is estimated at 3.8 per 100,000; more common in females (F:M ~9:1). The disease course may evolve toward a predominance of one specific connective tissue disease phenotype over time.
Mixed Connective Tissue Disease (MCTD): A distinct autoimmune condition with overlapping features of SLE, SSc, and polymyositis, and high anti-U1 RNP antibodies.
Anti-U1 RNP antibodies: Autoantibodies targeting U1 small nuclear ribonucleoprotein complex; hallmark of MCTD.
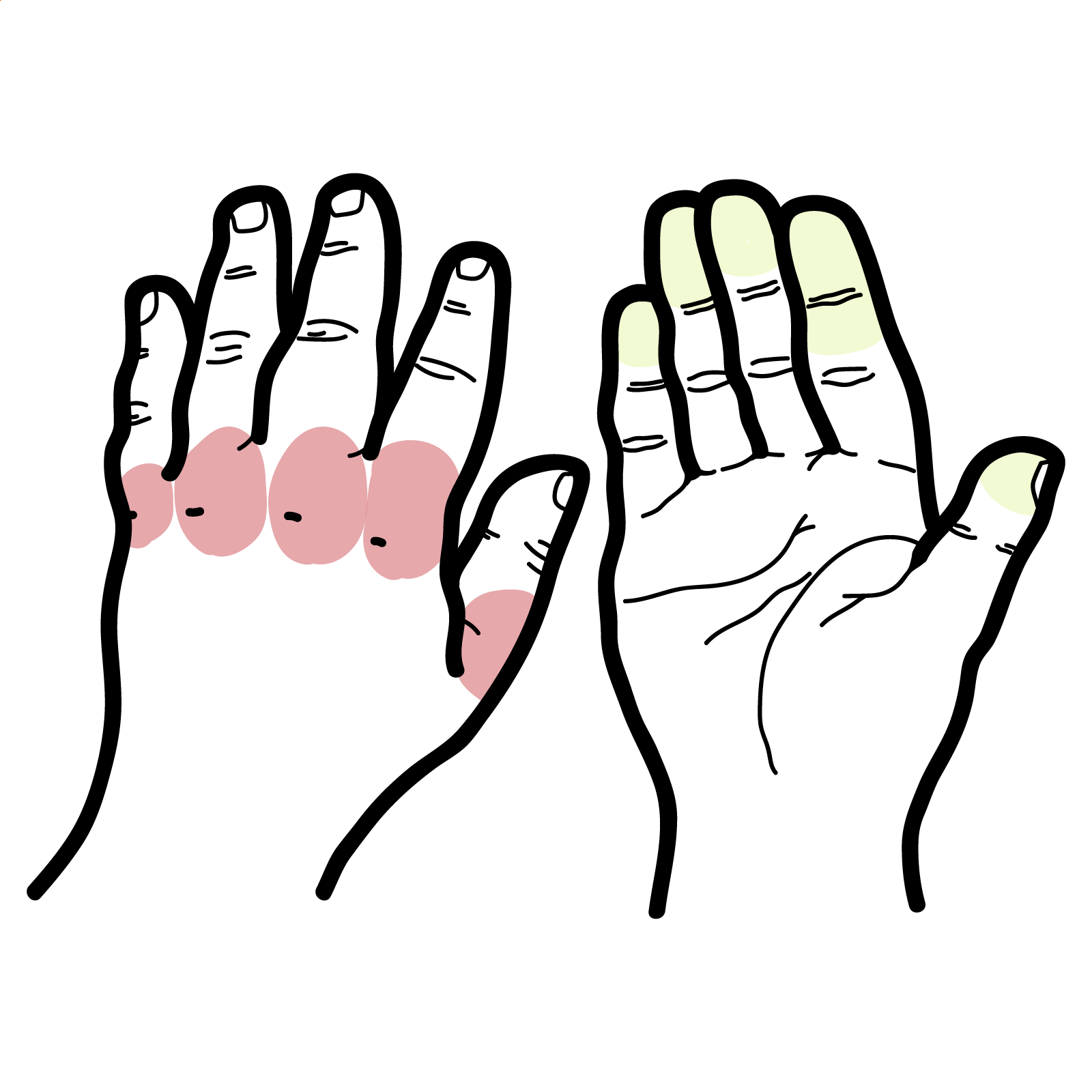
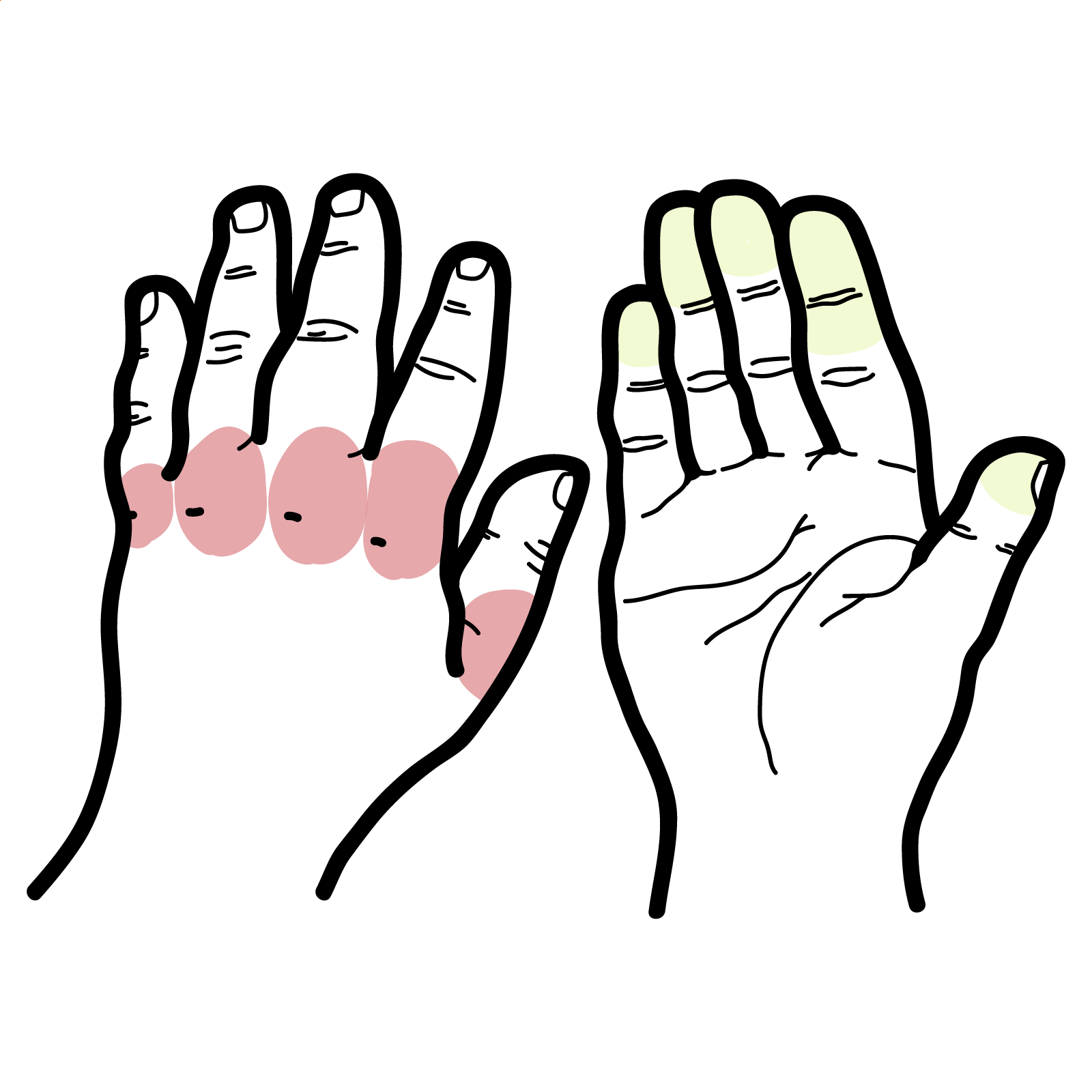
Raynaud’s phenomenon: Episodic digital ischemia triggered by cold/stress causing triphasic color change (white-blue-red).
Anti-U1 RNP not only aids in diagnosis but may drive immune complex deposition and systemic effects.
Common Features mixture or overlap of the following:
Systemic Symptoms
Diagnostic Criteria (Alarcón-Segovia, 1987 – widely used):
Investigations:
Differential Diagnoses:
| Condition | Differentiating Features |
| SLE | dsDNA, anti-Sm, renal involvement more prominent |
| Systemic sclerosis | Scl-70, diffuse skin thickening |
| Polymyositis | No Raynaud’s or sclerodactyly |
| RA | Erosive arthritis, anti-CCP positivity |
High anti-U1 RNP titre with overlapping features is diagnostic and may correlate with disease activity.
Always screen for pulmonary hypertension in MCTD patients with breathlessness or abnormal PFTs
Mild disease (arthralgia, Raynaud’s):
Moderate-to-severe disease:
Pulmonary hypertension: endothelin receptor antagonists, sildenafil.
Poor Prognostic Factors
High corticosteroid requirement.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion