Overview
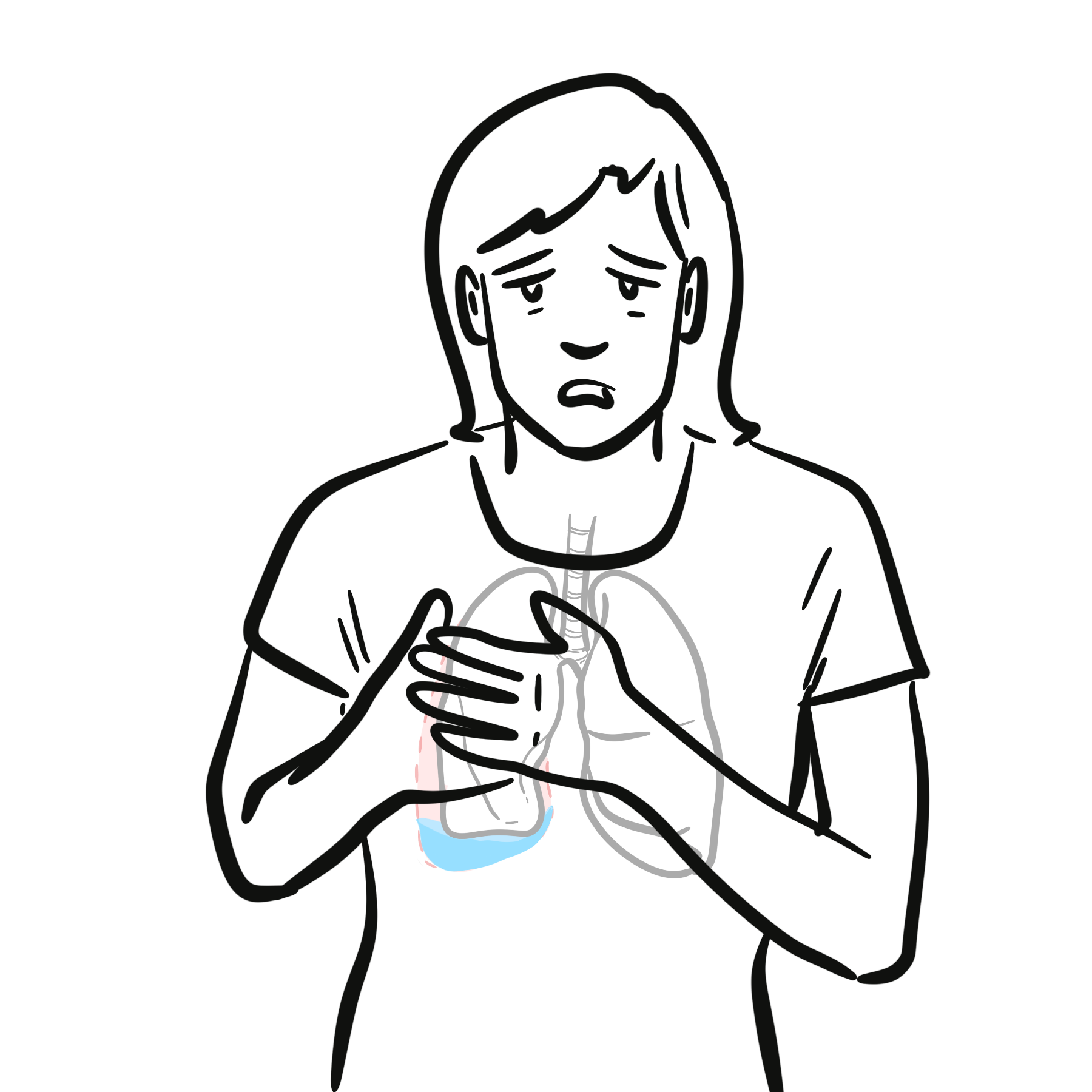
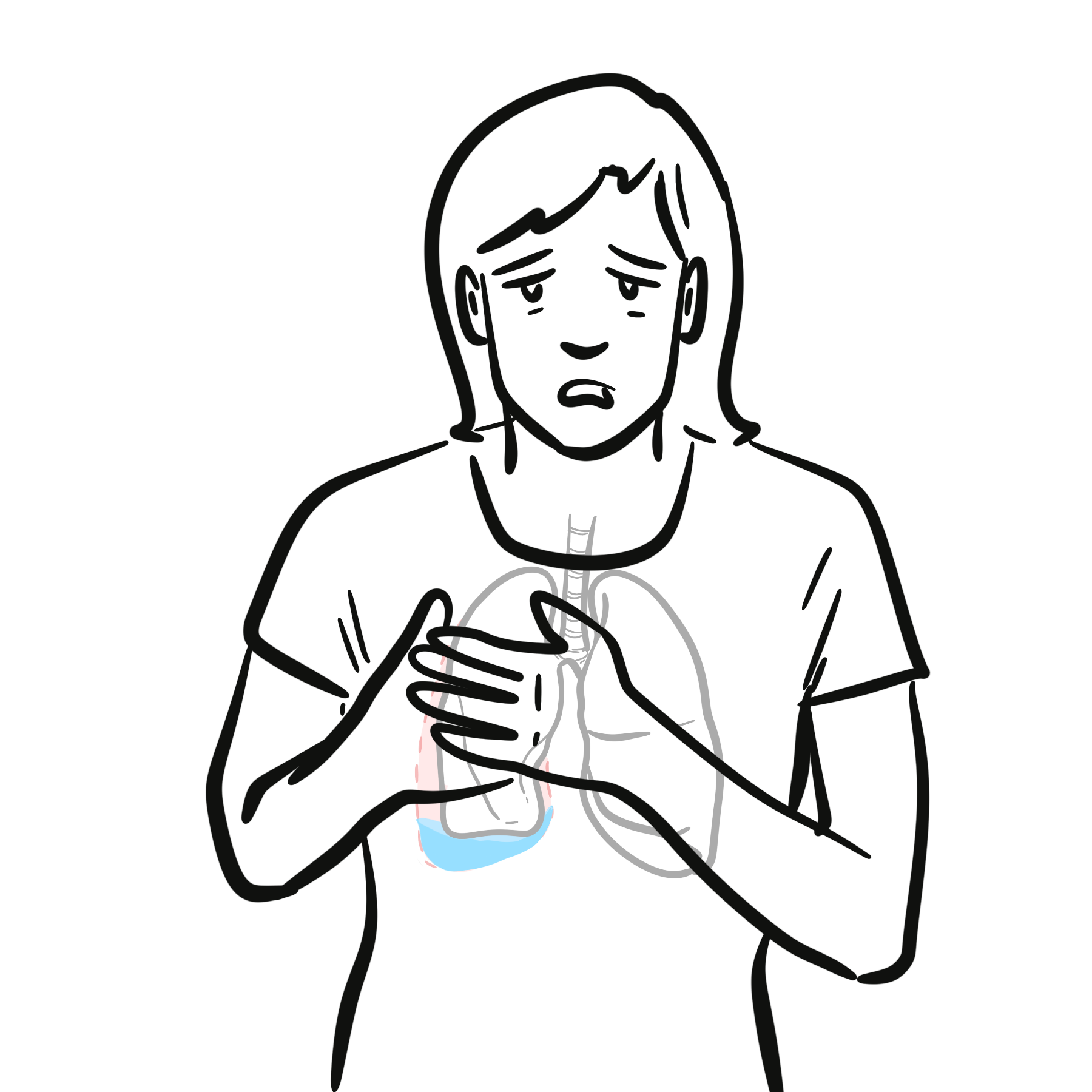
Rheumatoid pleural effusion (RPE) is an uncommon extra‑articular manifestation of rheumatoid arthritis (RA), occurring in ~2–5% of patients, more often in middle‑aged men with high rheumatoid factor (RF) titres, despite RA being more common in women. It typically presents during active disease or in patients with rheumatoid nodules, but can occasionally precede joint symptoms. RPE is usually unilateral, exudative, and associated with very low pleural fluid glucose and pH. Complications include pleural thickening, trapped lung, and chronic fibrothorax.
Although RA is more common in women, RPE is more frequent in middle‑aged men with high RF titres. Typically unilateral.
Definition
Rheumatoid pleural effusion (RPE): Exudative pleural effusion secondary to pleural involvement by RA.
Exudate: Pleural fluid meeting Light’s criteria for high protein and LDH content.
Trapped lung: Inability of lung to expand due to fibrous visceral pleural peel.
Pleural thickening: Fibrotic change of pleura following inflammation.
Anatomy & Physiology
- Pleura: Visceral pleura covers lung surface; parietal pleura lines thoracic cavity.
- Pleural space: Potential space with small amount of lubricating fluid.
- Fluid dynamics: Balance between hydrostatic, oncotic pressures, and lymphatic drainage maintains minimal pleural fluid.
Aetiology and Risk Factors
Aetiology
- Direct pleural involvement by rheumatoid inflammation.
- Immune complex deposition in pleura → complement activation → inflammation.
Risk Factors
- Male sex (despite RA being more common in females).
- Age 40–60 years.
- High RF titres.
- Long‑standing, seropositive RA.
- Presence of rheumatoid nodules.
- Smoking.
Pathophysiology
- Immune dysregulation in RA → autoantibody production (RF, anti‑CCP).
- Immune complex deposition in pleura.
- Complement activation → neutrophil recruitment.
- Pleural inflammation → increased vascular permeability.
- Exudative effusion formation with biochemical changes:
- ↓ glucose (due to high metabolic activity of inflammatory cells).
- ↓ pH (due to lactic acid production).
- ↑ LDH (cell breakdown).
Clinical Manifestations
- Often asymptomatic; detected incidentally.
- Dyspnoea, pleuritic chest pain, cough.
- Signs: Dullness to percussion, ↓ breath sounds, ↓ tactile fremitus on affected side
RPE can precede joint symptoms in rare cases.
Diagnosis
- Pleural fluid analysis
- Exudate by Light’s criteria.
- Very low glucose (<30 mg/dL).
- Low pH (<7.2).
- High LDH (>700 IU/L).
- High RF titre in pleural fluid.
- Cytology: Predominantly lymphocytes; absence of malignant cells.
- Imaging
- CXR – unilateral effusion
- US – guides thoracentesis
- CT – pleural thickening.
- Differential Diagnosis
- Parapneumonic effusion – higher glucose, neutrophil predominance.
- Tuberculous pleuritis – lymphocytic, high ADA.
- Malignant effusion – positive cytology.
In a patient with unexplained exudative effusion and very low glucose, always consider RA, TB, and empyema.
RA related pleural effusion biochemical signature: very low glucose, low pH (<7.2), high LDH (>700 IU/L) and high RF titre in pleural fluid → This combination is highly suggestive of RPE.
Tuberculous pleuritis can mimic RPE biochemistry except for ADA elevation in TB — always check ADA in endemic areas.
Treatment
- Asymptomatic/small effusions: Observation; treat underlying RA.
- Symptomatic/large effusions: Therapeutic thoracentesis.
- Recurrent/persistent effusions:
- Optimise RA control (DMARDs, biologics).
- Corticosteroids (systemic or intrapleural in select cases).
- Pleurodesis or decortication for trapped lung.
- Supportive: Analgesia, pulmonary rehab if chronic impairment.
Antibiotics are not indicated unless secondary infection is suspected.
Complications and Prognosis
Complications
- Pleural thickening.
- Trapped lung.
- Chronic fibrothorax.
- Secondary infection/empyema.
Prognosis
- Many resolve with RA control.
- Chronic effusions may cause restrictive lung defect.
- Poor prognostic factors: trapped lung, recurrent large effusions, uncontrolled RA.
References
- Shaw M, et al. Rheumatoid arthritis-associated lung disease. Eur Respir Rev. 2015;24(135):1‑16.
- Sivakumaran Y, et al. Rheumatoid pleuritis. Aust Fam Physician. 2015;44(11):829‑831.
- Stout J, et al. Rheumatoid pleural effusions and trapped lung. Am J Hosp Med. 2015;7(2):1‑4.
- Light RW. Pleural Diseases. 7th ed. Wolters Kluwer; 2018.

Discussion