Reactive Arthritis
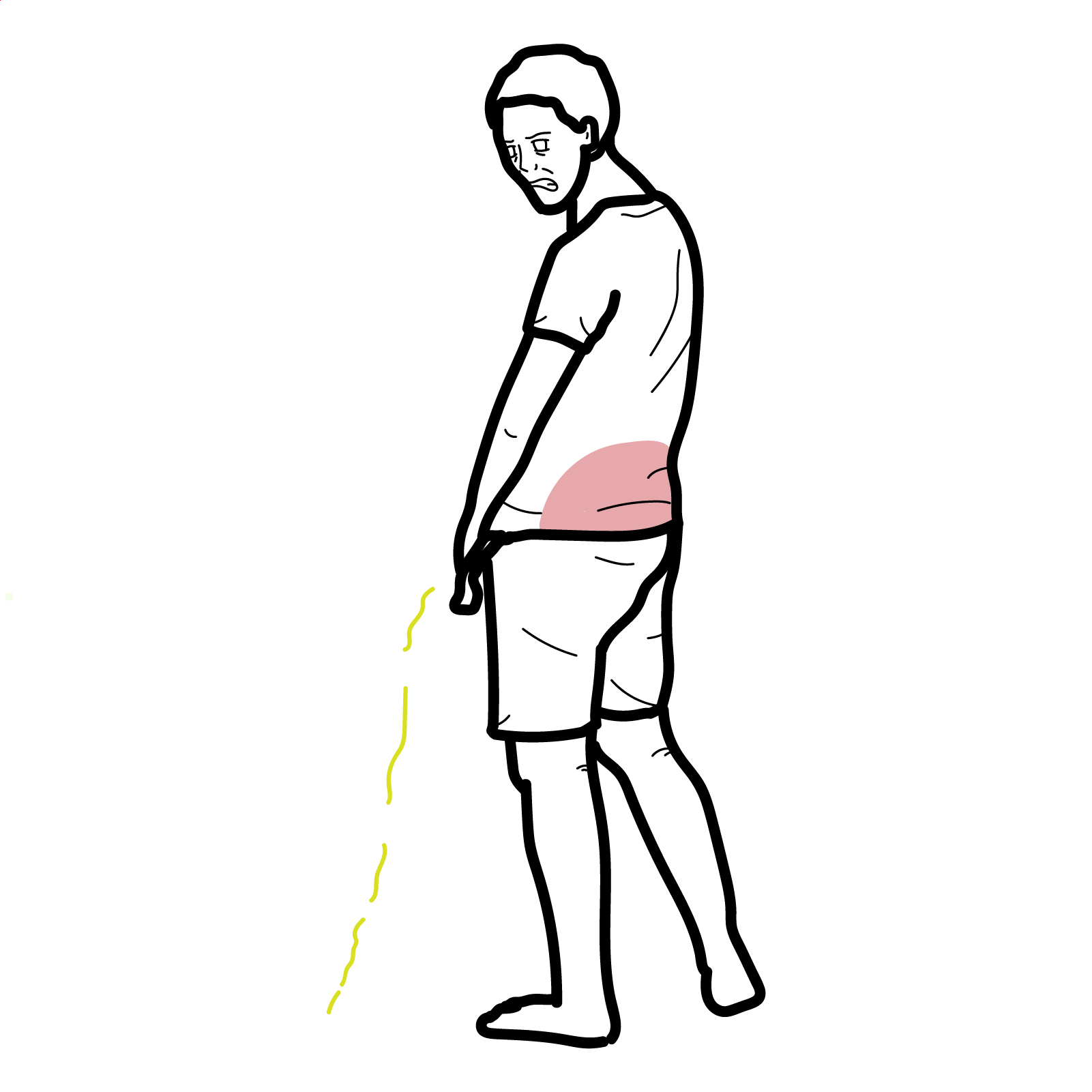
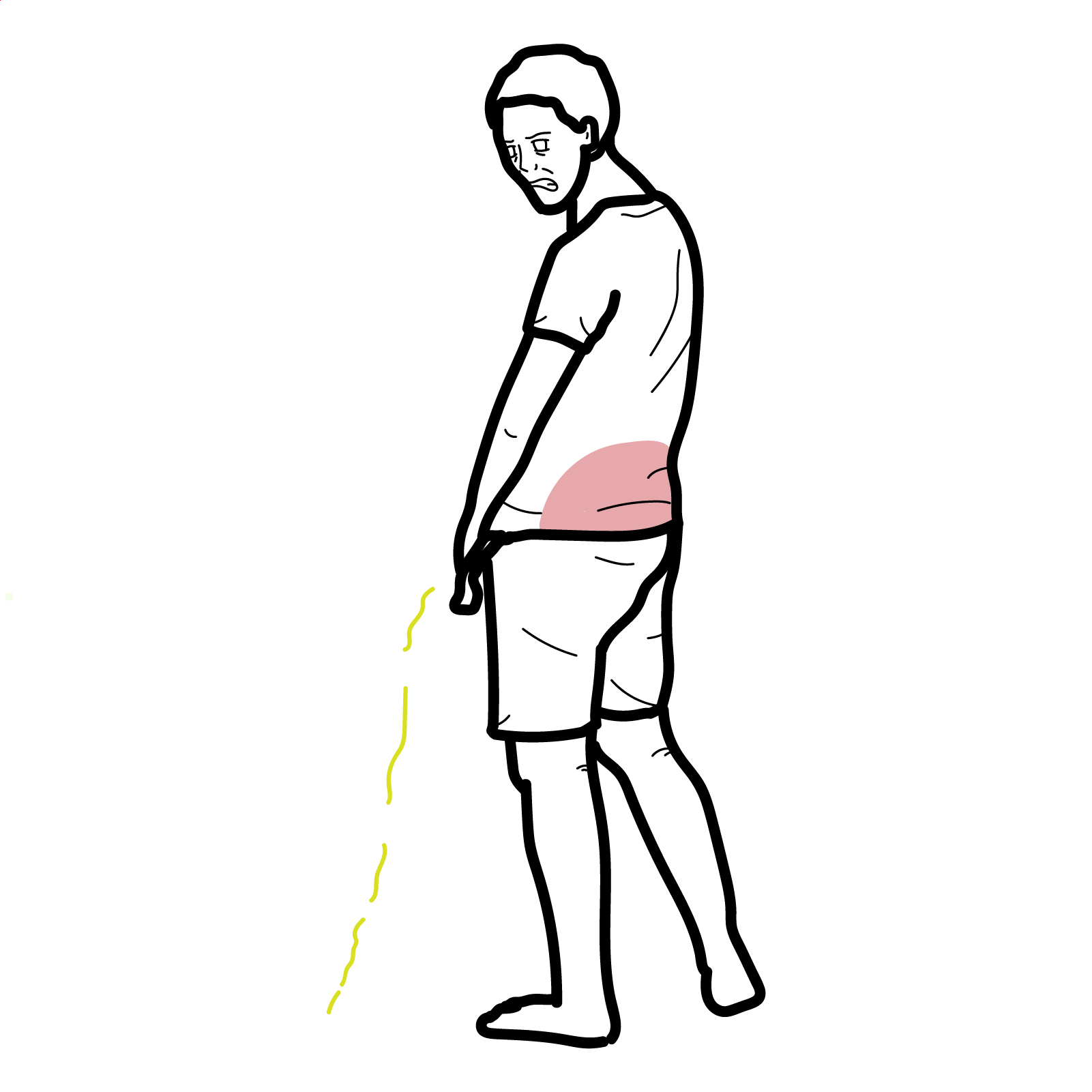
Reactive arthritis is a seronegative spondyloarthropathy that occurs after a genitourinary or gastrointestinal infection, typically presenting as an asymmetric oligoarthritis, often with associated conjunctivitis and urethritis (formerly Reiter’s syndrome). It most commonly affects young adults aged 20–40 and shows a strong association with HLA-B27. Incidence is estimated at 30–40 per 100,000, with higher rates in HLA-B27–positive individuals following infection.
Reactive arthritis: Sterile inflammatory arthritis occurring 1–6 weeks after infection.
Seronegative spondyloarthropathy: Group of inflammatory arthritides negative for RF/anti-CCP.
Enthesitis: Inflammation at sites of tendon/ligament insertion.
Dactylitis: Diffuse swelling of an entire digit due to synovitis and tenosynovitis.
Always ask about recent diarrhoea, dysuria, or STI symptoms in young patients with new arthritis.
Arthritis in ReA is sterile — no live organisms are found in the joint.
Triad: Arthritis, conjunctivitis, urethritis (Reiter’s syndrome — classic but rare today).
No dedicated ReA classification criteria. Often diagnosed clinically based on:
– Acute oligoarthritis
– Preceding GI/GU infection
– Absence of live pathogen in joint fluid
Differential Diagnoses:
| Condition | Differentiating Features |
| Septic arthritis | Fever, single joint, positive culture |
| Gonococcal arthritis | Young sexually active adults, migratory arthritis, tenosynovitis, skin pustules. Positive culture. |
| Viral Arthralgia | Joint pain without swelling following viral illness |
| Gout | Crystals in joint aspirate, often 1st MTP |
| Psoriatic arthritis | Skin/nail psoriasis, symmetric or axial involvement |
| IBD-related arthritis | History of Crohn’s/UC, gut symptoms |
Negative joint cultures + history of recent infection = key to diagnosis.
Chronic/refractory disease
Supportive: Physiotherapy, sexual health counselling, patient education
Treat the infection first if active; otherwise focus on joint symptoms.
Poor Prognostic Factors

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion