Sjögren’s Syndrome
Sjögren’s Syndrome is a chronic, systemic autoimmune disorder characterized by lymphocytic infiltration and destruction of exocrine glands, primarily affecting the salivary and lacrimal glands, leading to dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca). It commonly affects middle-aged women, with a female:male ratio of approximately 9:1. It can be primary (isolated) or secondary (associated with other autoimmune diseases like RA or SLE).
Sjögren’s Syndrome (SS): Autoimmune disease targeting exocrine glands, especially lacrimal and salivary.
Xerostomia: Dry mouth due to decreased salivary flow.
Keratoconjunctivitis sicca: Dry eyes from decreased tear production.
Extraglandular manifestations: Systemic features such as arthritis, neuropathy, ILD, and vasculitis.
Lacrimal glands produce tears to lubricate the eye and protect the cornea.
Salivary glands (parotid, submandibular, sublingual) produce saliva for digestion and oral health.
Exocrine glands are regulated by parasympathetic nervous system and rely on intact glandular epithelium for secretion.
Aetiology:
• Unknown, likely multifactorial
• Genetic predisposition (HLA-DR52, HLA-DR3)
• Environmental triggers (e.g. viral infections: EBV, CMV, HTLV-1)
• Aberrant activation of innate and adaptive immune system
Risk Factors:
• Female sex (90% of cases)
• Age 40–60
• Family history of autoimmune disease
• Coexisting autoimmune diseases (RA, SLE, scleroderma)
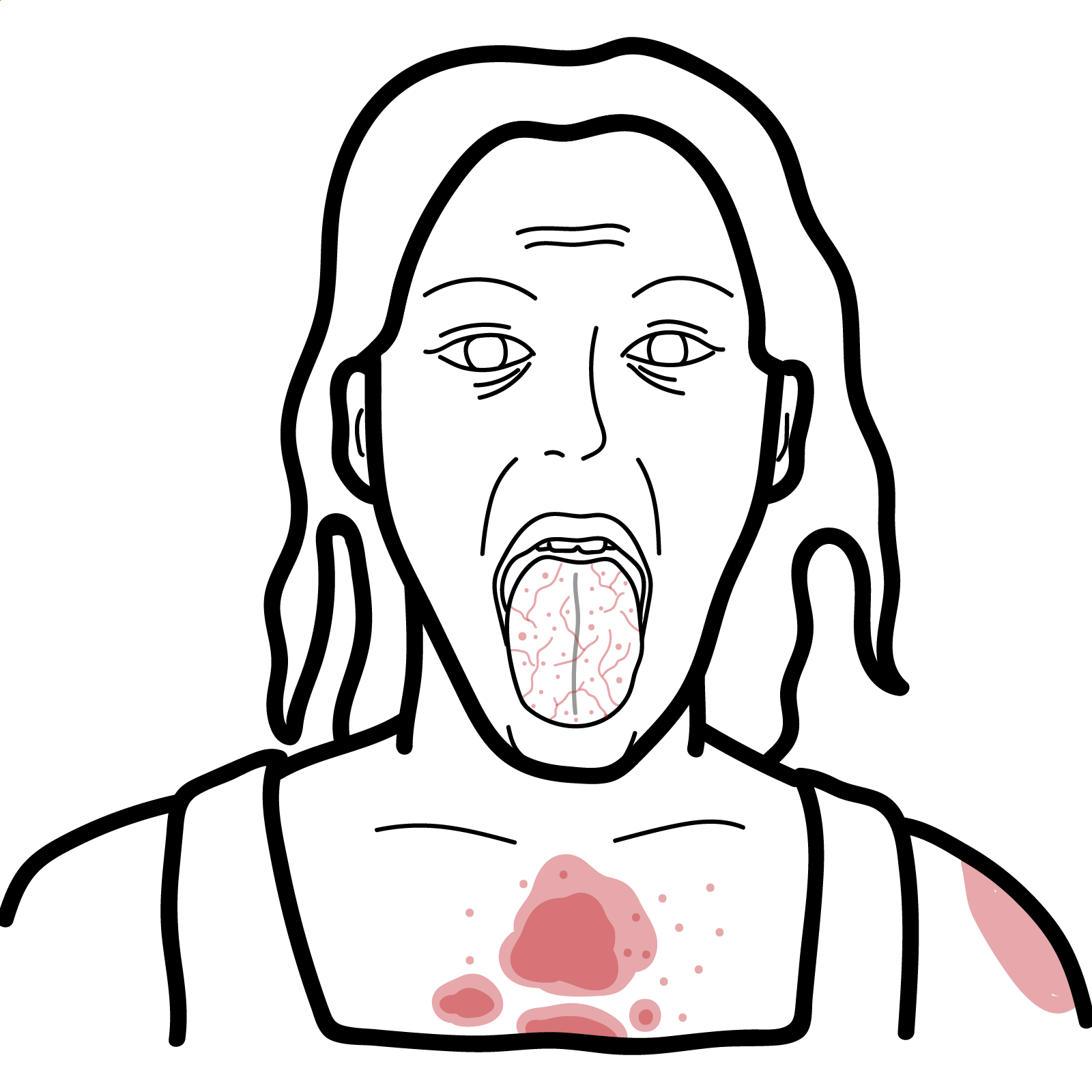
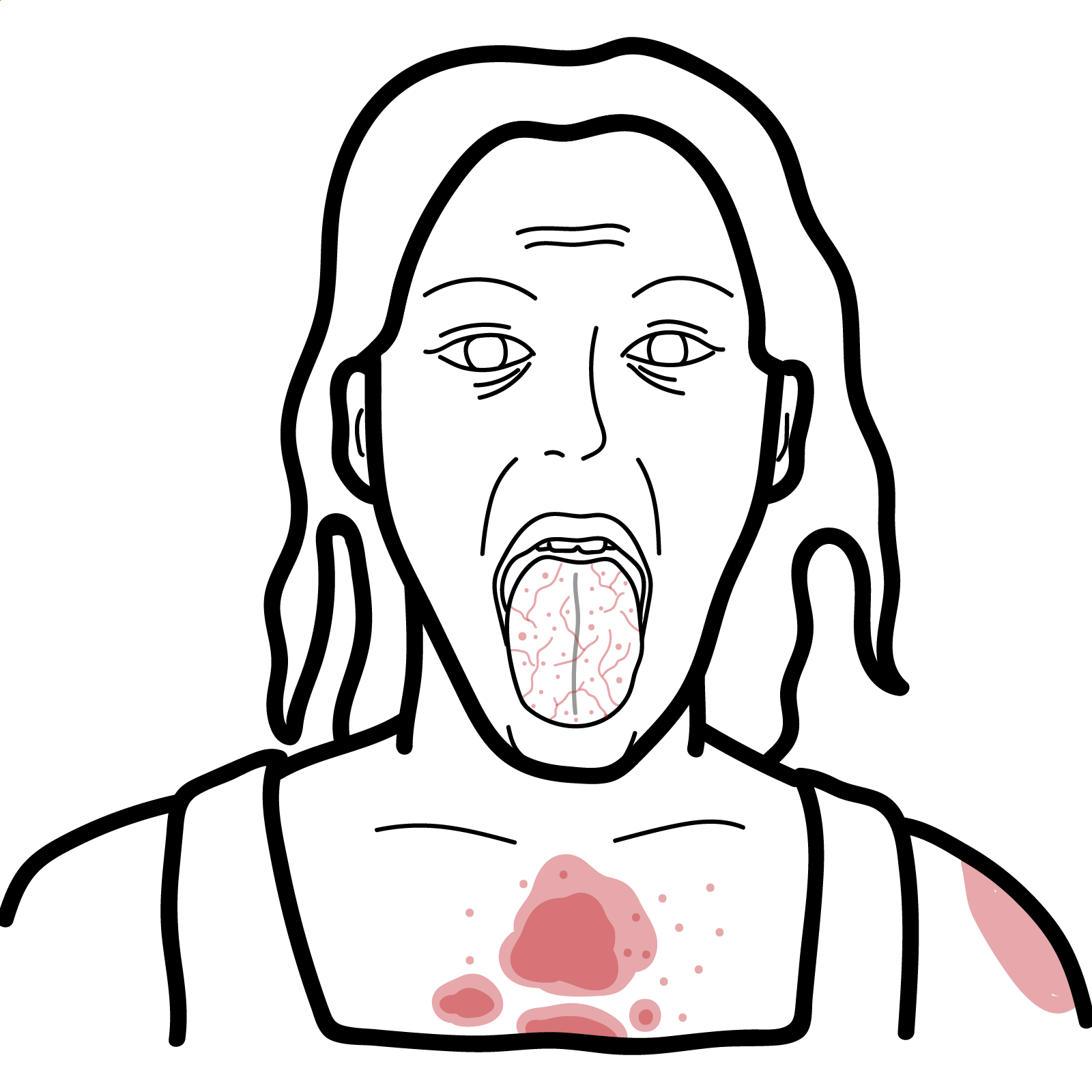
Glandular
• Xerostomia – difficulty swallowing, speaking, dental caries
• Keratoconjunctivitis sicca – gritty eye sensation, redness, photophobia
• Parotid enlargement – often bilateral and non-tender
Extraglandular (systemic)
• Arthralgia/arthritis – non-erosive, symmetric
• Interstitial lung disease
• Raynaud’s phenomenon
• Peripheral neuropathy
• Cutaneous vasculitis (palpable purpura)
• Renal involvement (distal RTA, interstitial nephritis)
• Fatigue
Triad: Xerostomia, Keratoconjunctivitis sicca, Parotid gland swelling
Sjogrens causes RTA Type I: A urine pH >5.5 in the setting of metabolic acidosis and hypokalemia is highly suggestive of type 1 RTA.
| Feature | Points |
| Positive anti-Ro/SSA antibodies | 3 |
| Labial salivary gland biopsy (focal lymphocytic sialadenitis with focus score ≥1) | 3 |
| Ocular staining score ≥5 (or van Bijsterveld ≥4 in at least one eye) | 1 |
| Schirmer’s test ≤5 mm/5 min in at least one eye | 1 |
| Unstimulated salivary flow rate ≤0.1 mL/min | 1 |
Differential diagnoses
| Feature | Anti-Ro (SSA) | Anti-La (SSB) |
| Prevalence in Sjögren’s | 60–75% | 40–50% |
| Sensitivity | Higher | Lower |
| Specificity | Moderate | Higher |
| Seen in other diseases | Yes (SLE, neonatal lupus) | Mostly limited to Sjögren’s |
| Clinical associations | ILD, vasculitis, neonatal lupus | Milder disease course |
Ro52 is found in autoimmune ILD conditions (SSc, RA) and typically associated with a poor prognostic factor.
Anti-Ro is highly sensitive, anti-La is more specific.
Glandular symptoms
Systemic/extraglandular
Tailor treatment to manifestations — not all patients need immunosuppression.
Poor Prognostic Factors
Any new lymphadenopathy or weight loss in SS → evaluate for lymphoma.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion