Takayasu Arteritis
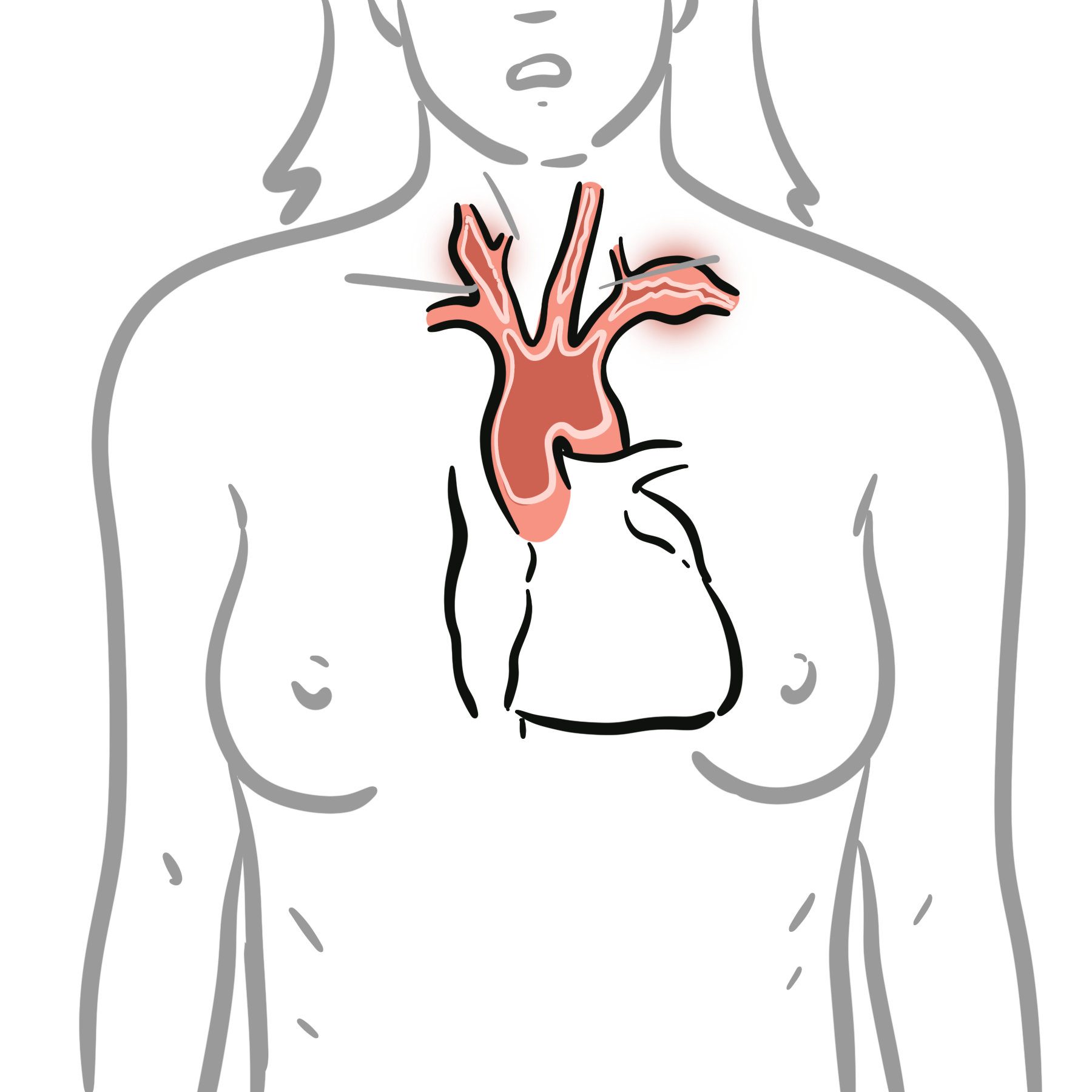
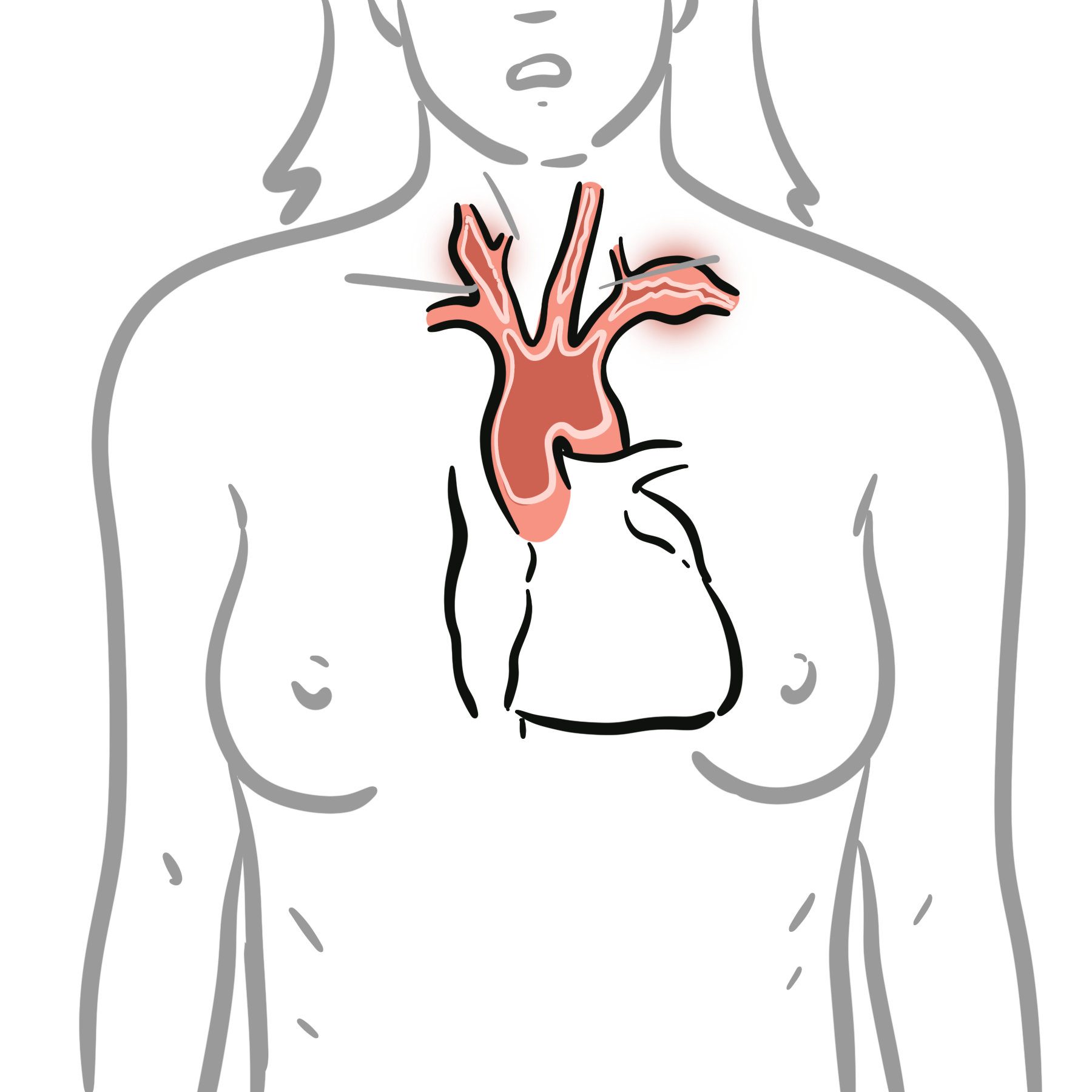
Takayasu arteritis is a rare, chronic large-vessel vasculitis primarily affecting the aorta and its major branches, leading to stenosis, occlusion, or aneurysm formation. It most commonly affects young women (<40 years), particularly of Asian descent. The global incidence is estimated at 1–2 per million per year, with a female predominance (F:M ~9:1). It is also called “pulseless disease” due to the hallmark feature of absent peripheral pulses in late-stage disease.
Takayasu arteritis is named after Mikito Takayasu, a professor of ophthalmology at Kanazawa University in Japan, who, in 1905, presented a case of a 21-year-old woman with wreath-like retinal vascular anastomoses at the Annual Meeting of the Japanese Ophthalmology Society.
Stenosis: Narrowing of a vessel, reducing blood flow.
Bruits: Audible vascular turbulence over narrowed vessels, a hallmark in TA.
Subclavian and carotid artery involvement often explains neurological and upper limb symptoms in TA.
TAK is a panarteritis, but the initial site of inflammation is around the vasa vasorum and at the medio-adventitial junction. Large and medium-sized arteries are considered immune-privileged sites. Vascular dendritic cells, located near the vasa vasorum, function as gatekeepers by restricting lymphocyte entry and dampening local immune-inflammatory responses.
The phase of inflammation (active vs fibrotic) impacts treatment and imaging findings.
Takayasu arteritis most commonly presents in young women under 40–50 years of age, particularly of Asian descent. Early Takayasu arteritis often goes undiagnosed because clinical features are nonspecific, but progression is associated with obstructive or aneurysmal lesions.
In addition to constitutional manifestation symptoms are related to the severity of specific arterial involvement.
| Phase | Description |
| Systemic (Pre-pulseless) phase | Non-specific inflammatory symptoms, mimicking infection or autoimmune disease |
| Occlusive (Vascular) phase | Ischemic symptoms due to progressive arterial stenosis or occlusion |
| Artery Involved | Clinical Manifestations |
| Subclavian artery | Upper limb claudication, asymmetric BP, subclavian steal syndrome |
| Carotid artery | Amaurosis fugax/Takayasu retinopathy (ophthalmic artery) TIA/stroke, carotidynia, cervical bruit |
| Vertebral artery | Posterior circulation TIA, vertigo, ataxia |
| Aortic arch/thoracic aorta | Pulse deficits, aortic regurgitation, thoracic bruit |
| Abdominal aorta | Mesenteric ischemia (intestinal angina), lower limb claudication, bruit |
| Renal arteries | Renovascular hypertension, hypertensive encephalopathy, CKD |
| Coronary arteries | Angina, myocardial infarction |
| Pulmonary arteries | Pulmonary hypertension, dyspnea, hemoptysis |
Suspect Takayasu in young female with unexplained hypertension, arm claudication, or pulse deficits.
Examination findings
Always check bilateral BP in young women with claudication or unexplained hypertension.
| Classification Criteria for Takayasu Arteritis (2022 ACR/EULAR) | ||
| Category | Feature | Points |
| Absolute Requirements | Age ≤ 60 years at time of diagnosis | Required |
| Evidence of vasculitis in the aorta or its branches on imaging | Required | |
| Additional Clinical Criteria | Female sex | +1 |
| Angina or ischemic cardiac pain | +2 | |
| Arm or leg claudication | +2 | |
| Vascular bruit over aorta or major arteries | +2 | |
| Reduced or absent pulse in upper extremity (axillary, brachial, or radial arteries) | +2 | |
| Carotid artery abnormality on imaging | +2 | |
| Systolic blood pressure difference ≥ 20 mm Hg between arms | +1 | |
| Additional Imaging Criteria | One affected arterial territory | +1 |
| Two affected arterial territories | +2 | |
| Three or more affected arterial territories | +3 | |
| Symmetric involvement of paired arteries (e.g., bilateral carotid or renal arteries) | +1 | |
| Abdominal aorta involvement with either renal or mesenteric arteries | +3 | |
| Diagnosis = Total score ≥ 5 | ||
Differential Diagnoses:
| Condition | Differentiators |
| Giant cell arteritis | Age >50, temporal artery involvement |
| Atherosclerosis | Older age, risk factors, calcifications |
| Fibromuscular dysplasia | String-of-beads appearance, no systemic symptoms |
| Coarctation of aorta | Congenital, BP difference in upper vs lower limbs |
Based on angiographic pattern (Numano classification):
| Type | Involvement |
| I | Aortic arch and branches |
| IIa | Ascending aorta, arch, branches |
| IIb | IIa + thoracic descending aorta |
| III | Thoracic + abdominal aorta |
| IV | Abdominal aorta, renal arteries |
| V | Entire aorta and branches |
Most patients have Type V, with widespread arterial involvement.
| Phase | Treatment |
| Active inflammation | High-dose corticosteroids (prednisolone 1 mg/kg/day) |
| Steroid-sparing | Methotrexate, azathioprine, mycophenolate mofetil |
| Refractory | Biologics (e.g. tocilizumab, TNF inhibitors) |
| Vascular complications | Revascularization (angioplasty or bypass) after controlling inflammation |
Monitoring: ESR/CRP, imaging every 6–12 months.
Treat inflammation aggressively before vascular repair to reduce restenosis.
Complications
Poor Prognostic Factors

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion