Overview
Pelvic inflammatory disease (PID) comprises a spectrum of inflammatory disorders of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. Causative organisms are either sexually transmitted (such as C trachomatis, N gonorrhoeae, Mycoplasma genitalium) or endogenous vaginal organisms (for example, Bacteroides species) that ascend into the pelvic area from the lower genital tract through the cervix. Pelvic inflammatory disease is a major concern because it can result in longterm reproductive disability, including infertility, ectopic pregnancy, and chronic pelvic pain.
| Definition Pelvic Inflammatory Disease: Inflammation and infection of the upper genital tract in women, typically involving the uterus and adnexa Mild to moderate PID: Absence of a tubo-ovarian abscess Severe PID: Severe systemic symptoms or the presence of a tubo-ovarian abscess |
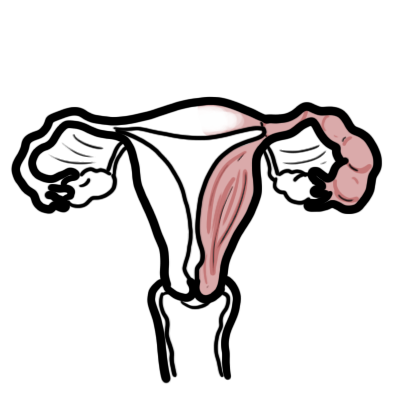
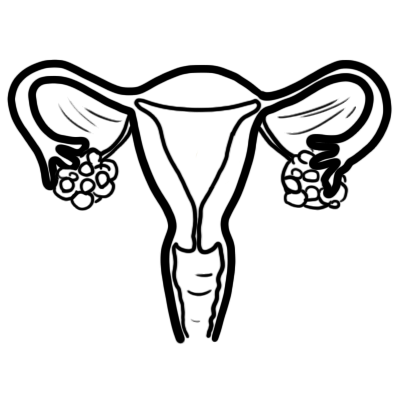
Anatomy and Physiology
Vaginal Microbiology
The hydrogen peroxide-producing Lactobacillus species is the most dominant, non-pathogenic organism living in the vagina. The vaginal flora of most normal, healthy women also includes a variety of potentially pathogenic bacteria in low numbers:
- Streptococci
- Staphylococci
- Enterobacteriaceae (most commonly Klebsiella spp, Escherichia coli, and Proteus spp)
Many factors influence the vaginal microflora including:
- Hormonal changes (eg, pregnancy, menstrual cycle)
- Contraceptive method
- Sexual activity
- Other unknown factors
Cervix
The endocervical canal functions as a barrier protecting the normally sterile upper genital tract from the organisms of the dynamic vaginal ecosystem. Endocervical infection with sexually transmitted pathogens can disrupt this barrier.
Risk Factors
- Young age
- Low socioeconomic status
- Lower educational attainment
- Recent new sex partner.
- Prior STI
- Young age at onset of sexual activity
- Unprotected sexual intercourse with multiple partners
- Sex during or just after menstruation
- History of PID
- Alcohol/Illicit drug use
- Genetic and Immunological factors
Signs and Symptoms
PID is mostly asymptomatic
Acute PID: characterized by the acute onset of lower abdominal or pelvic pain, pelvic organ tenderness, and evidence of inflammation of the genital tract.
Subclinical PID: Subclinical infection of the upper reproductive tract that does not prompt a woman to present to medical care but is severe enough to produce significant sequelae appears to be relatively common.
Chronic PID: An indolent presentation of PID with low-grade fever, weight loss, and abdominal pain has been reported with actinomycosis and tuberculosis.
Differential Diagnosis
| Condition | Clinical Features |
| Ectopic pregnancy | History of missed menses, positive pregnancy test |
| Ovarian cyst rupture/torsion | Sudden onset of severe pain |
| Endometriosis | Cyclical or chronic pain |
| Cystitis | Urinary frequency and/or dysuria |
| Appendicitis | Pain localized to the right iliac fossa, vomiting |
| Diverticulitis | Bowel symptoms in older women |
| Irritable bowel syndrome | Generalized abdominal pain, constipation, diarrhea |
| Functional pain | Other causes have been excluded |
Investigations
- FBC
- ESR
- Nucleic acid amplification tests – Chlamydia or Gonorrhoea
- Saline microscopy – Trichomonas vaginalis infection or bacterial vaginosis
- Transvaginal ultrasound
- CT
- Endometrial biopsy
- Laproscopy – gold standard (invasive maybe only for severe cases)
Diagnosis
One or more of the following minimum criteria must be present on pelvic examination to diagnose PID:
- Cervical motion tenderness
- Uterine tenderness
- Adnexal tenderness
The following criteria can improve the specificity of the diagnosis:
- Fever
- Abnormal Vaginal Discharge
- Presence of abundant numbers of white blood cells on saline microscopy of vaginal fluid
- ↑ Erythrocyte sedimentation rate
- Laboratory documentation of cervical infection with gonorrhea or chlamydia
The following test results are the most specific criteria for diagnosing PID:
- Endometrial biopsy – endometritis
- Transvaginal sonography or magnetic resonance imaging techniques showing thickened, fluid-filled tubes +/- free pelvic fluid or tubo-ovarian complex
- Doppler studies
- Laparoscopy
Aetiology
Pelvic inflammatory disease (PID) is a polymicrobial infection of the upper genital tract that primarily affects young, sexually active women. In most cases, the precise microbial etiology of PID is unknown. When known:
- STI pathogens or bacterial vaginosis (85% of cases)
- Neisseria gonorrhoeae (Most common)
- Chlamydia trachomatis (Most common)
- Mycoplasma genitalium
- Bacterial Vaginosis (gardenlla vaginalis)
- Respiratory or enteric organisms that have colonized the lower genital tract (15%)
- Streptococci
- Staphylococci
- Enterobacteriaceae (most commonly Klebsiella spp, Escherichia coli, and Proteus spp)
- Rare: Mycobacterium tuberculosis and the agents of actinomycosis
Pathophysiology
- Ascending infection from the cervix is often due to sexually acquired infections
- Infection moves from cervix→ fallopian tubes → peritoneal surface of the fallopian tubes → ovaries
- Infection results in fibrinous or suppurative inflammatory damage along the epithelial surface of the reproductive tract
- This leads to scarring, adhesions, and possibly partial or total obstruction of the fallopian tubes.
- Reinfection substantially increases the risk of tubalfactor infertility
- The inability to conceive because of structural or functional damage to the fallopian tubes
- The adaptive immune response thought to play a role in this
- Infection-induced selective loss of ciliated epithelial cells along the fallopian tube epithelium can cause impaired ovum transport
- This results in tubal-factor infertility or ectopic pregnancy
- Peritoneal adhesions along the fallopian tubes may prevent pregnancy, and adhesions within the pelvis are related to pelvic pain.
| Side note PID can occur after instrumentation of the uterus, such as during D & C for termination of pregnancy or miscarriage, or insertion of an PID. |
| Side note PID can be caused by polyps, fibroids and neoplasms, which prevent closure of the uterine cavity and allow endogenous organisms to colonise the upper genital tract. |
The microorganisms that are implicated in PID are thought to spread in three ways:
- Intra-abdominally, traveling from the cervix to the endometrium, through the salpinx, and into the peritoneal cavity (causing endometritis, salpingitis, tubo-ovarian abscess, or pelvic peritonitis)
- Through the lymphatic systems, such as infection of the parametrium from an intrauterine device (IUD)
- Through hematogenous routes, such as with tuberculosis (rare)
Management
Empiric antibiotic treatment should be initiated at the time of presentation in patients with symptoms suspicious for PID, even if the diagnosis has not been confirmed. Antibiotics can be any of the following depending on severity and situation:
- Parenteral Antibiotics
- Oral Antibiotics
- IV Antibiotics
Remember to test and treat the partner if necessary. Partners should be instructed to abstain from sexual intercourse until they and their sex partners have been adequately treated.
Mild to moderate (outpatient) Oral antibiotics
- Ceftriaxone PLUS Doxycycline PLUS Metronidazole PLUS Azythromycin
Severe (Inpatient) IV Antibiotics
- Ceftriaxone PLUS Cefotaxime PLUS Metronidazole PLUS Azythromycin
Follow up
- If no improvements after 3 days reassess +/- hospitalisation
- Remove intrauterine device (IUD) if no response to treatment in 48-72 hours.
- If Chlamydia or gonococcal infection retest in 3 months
| Indications for hospitalzation |
| Inability to follow or tolerate an outpatient oral medication regimen |
| Pregnancy |
| No clinical response to oral antimicrobial therapy |
| Severe illness, nausea and vomiting, or high fever |
| Severe illness, nausea and vomiting, or high fever |
| Surgical emergencies (e.g., appendicitis) cannot be excluded |
| Tubo-ovarian abscess |
| Remember Pregnant women suspected to have PID are at high risk for maternal morbidity and preterm delivery. These women should be hospitalized and treated with intravenous antibiotics. |
| Side note Screening for lower genital tract chlamydial infection in younger and high-risk populations is recommended to reduce the incidence of PID. Asymptomatic disease should be treated. |
Complication and Prognosis
Complications (I-FACE-PID)
- Infertility
- Fitz-Hugh-Curtis syndrome
- Abscesses
- Chronic pelvic pain
- Ectopic pregnancy
- Peritonitis
- Intestinal obstruction
- Disseminated infection (sepsis, endocarditis, arthritis, meningitis)
Prognosis Patients who have co-existent conditions (HIV infection, pregnancy, IUD, prior PID or tubo-ovarian abscess) require close observation and may require hospitalisation.
- 20% of women with PID become infertile
- 40% develop chronic pain,
- 1% of those who conceive have an ectopic pregnancy
- Spontaneous resolution of symptoms may occur in some women.




Discussion