Overview
Premenstrual syndrome is defined as recurrent moderate psychological and physical symptoms that occur during the luteal phase of menses and resolve with menstruation. Most women of reproductive age experience one or more mild emotional or physical symptoms for one to two days before the onset of menses. These symptoms, such as breast soreness and bloating, are mild and do not cause severe distress or functional impairment, and are not considered to represent premenstrual syndrome.
| Definition PMS: Recurrent psychological or somatic symptoms (or both) occurring specifically during the luteal phase of the menstrual cycle and which resolve in the follicular phase at least by the end of mensutruation PMDD: Is the severe form of PMS in which symptoms of anger, irritability and internal tension are prominent. |
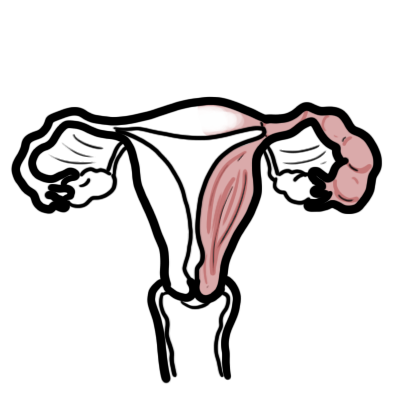
Physiology of Menstruation
| Watch Video Female Reproductive Cycle: Menstrual cycle |
Signs and Symptoms
Clinical Features
- Distressing psychological, physical and behavioral symptoms
- Occurs during luteal phase of the menstrual cycle
- Significant regression of symptoms with onset of or during the period (bleeding)
Physical Symptoms
- Abdominal bloating
- Body aches
- Breast tenderness and/or fullness
- Cramps, abdominal pain
- Fatigue
- Headaches
- Nausea
- Swelling of extremeties
- Weight gain
Psychological and behavioural
- Anger Irritability
- Anxiety
- Changes in appetitie
- Changes in libido
- Decreased concentration
- Depressed Mood
- Feeling out of control
- Modd Swings
- Poor sleeps
- Tension
Investigations and Diagnosis
No need for investigation unless something sinister is suspected. It is important to make sure the signs and symptoms experienced by the woman are not occurring out side the luteal phase of the menstrual cycle. Also it is important to rule out other organise diseaes and significant psychiatric illness.
Diagnosis Clinical history is key to the diagnosis of PMS or PMDD. Other affective disorders such as depression and anxiety may have premenstrual cyclic worsening, but do not have the symptom-free interval during the mid-follicular phase (days 6 through 10 of the menstrual cycle) needed for the clinical diagnosis of PMS or PMDD.
Pathophysiology
UNKNOWN
There do appear to be at least three components to the aetiology of PMS:
- A brain component
- An ovulatory menstrual cycle
- Psychosocial factors and other factors Women who suffer from severe
PMS commonly date their problems from a bout of postnatal depression. Also, they typically have depressive side effects from progestogens such as medroxyprogesterone acetate, norethisterone and levonorgestrel.
Management
Hormonal Treatment
- Combined Oral contraceptive pills
- GnRH analogues
Non-Hormonal
- SSRI/SNRIs
- TCA
| Remember Selective serotonin reuptake inhibitors are effective in relieving PMS symptoms. |
Self managing strategies
- Healthy diet
- Vitamins and Minerals
- Exercise
- Stress reduction (yoga, tai-chi)
- Cognitive Behavioural Therapy
- Acupuncture
- Herbal remedies
- Mind-body therapy (aromatherapy, reflexology, magnotherapy)
| Natural therapies that have positive evidence for the treatment of PMS |
| Vitamin B6 |
| Calcium |
| Magnesium |
| Evening Primose Oik |
| Premular (an extract of the berries form the chaste tree) |
| St John’s wart extract |
Prognosis
Women with PMS and PMDD who begin medical therapy should be monitored at least every 3 months for efficacy of the treatment. The need for treatment continuation should be reviewed regularly.
Pre-Menstrual Dysmorphic Syndrome
Overview PMDD is a severe form of PMS. It occyrs in 8% of woman who are having their menstrual cycle. Genetic factors may play a role (daughters of mothers with PMDD are likely to have the disorder as well, identical twins 93%).
Risk Factors
- Anxiety
- Major Depression
- Seasonal affective disorder
- Alcohol abuse
- Overweight
- Sedentary lifestyle
- Family history
Signs and Symptoms are similar to PMS, more severe. Occurs during the week before menstrual bleeding.
Diagnosis FIVE of more must be present for most of the late luteal phase with remission within a few days of onset of menses:
- Disinterest in ADLs
- Fatigue or low energy
- Suicidal thoughts
- Binge eating
- Panic attacks
- Headaches and/or joint or muscle pain
- Persistent irritability
- Sleeplessness
- Trouble concetrating
Treatment
- Balanced Diet
- Sufficient sleep
- Exercise
- Oral contraceptive pill
- Anti-depressants
- CBT




Discussion