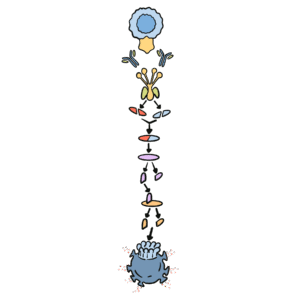
0:00 So, here we have the pathogen, a bacteria, for example, and it expresses a PAMP 0:10 , certain 0:11 PAMPs, and it has a special composition. 0:13 Now, the covalent protein can help in the phagocytizing process, so the coval 0:17 ent proteins 0:18 can bind to this pathogen as well. 0:22 And the macrophage can identify this pathogen either by receptors that 0:28 recognize the PAMP 0:29 such as a tall-like receptor, and it can also recognize the pathogen by the c 0:35 ovalent protein 0:36 on it, so with the covalent receptor recognizing the covalent protein on the 0:42 pathogen. 0:43 And so, with this, the macrophage can engulf this pathogen and form a phagosome 0:48 , not a 0:48 phagosome, this is an error here, and the macrophage also contains a lysosome, 0:54 which 0:54 has basically an acidic environment within it, with many enzymes such as hydrol 0:59 ases, 0:59 and this lysosome and phagosome will combine together to form a phagosome. 1:04 When it does this, the acidic environment will essentially destroy this path 1:10 ogen into small 1:10 bits and pieces, into small antigens as well. 1:13 Now, what good is this? 1:16 The macrophage can actually now take the antigen and express it on its cell 1:21 surface through 1:22 an MHC receptor, so therefore a macrophage is known as an antigen-presenting 1:29 cell. 1:30 With this, the macrophage can also stimulate the adaptive immune cells within 1:35 the lymph 1:36 node. 1:38 This is exactly the same as a dendritic cell. 1:41 The dendritic cell is also an antigen-presenting cell. 1:45 Now, the macrophage and dendritic cell, for example, once they have engulfed 1:52 this pathogen 1:53 and beginning to express it, it will start secreting cytokines as well to 1:59 enhance the 2:00 immune response. 2:01 The cytokines secreted by the macrophage and the dendritic cells are cytokines 2:08 CXCl8, which 2:09 attracts more leukocytes, also interleukin-6, which activates the lymphocytes, 2:18 the BMT 2:19 cell, and stimulates the liver to make more proteins for the immune response. 2:24 It will also secrete cytokines interleukin-1B, which increases vascular perme 2:30 ability, allowing 2:31 more leukocytes to enter the specific tissue, interleukin-12, which activates 2:37 the natural 2:38 killer cells and differentiation of a naive CD4 cell into a T helper-1 cell. 2:46 And finally, lastly, it also secreats tumor necrosis factor alpha, or TNF alpha 2:51 , which 2:52 is a pro-inflammatory cytokine, important in stimulating promoting the 2:57 inflammatory response. 2:58 Now, let's just concentrate on a macrophage again, specifically a macrophage, 3:02 not a dendritic 3:03 cell, but an activated macrophage, and see what it causes throughout the body 3:08 during 3:09 a pathogen invasion and infection, for example. 3:13 So activated macrophages to create cytokines, such as interleukin-1B, interleuk 3:16 in-6, and 3:17 TNF alpha. 3:18 So what does this do to different organs in the body and to our body itself? 3:24 Well, it will stimulate the liver for one, and it will stimulate the liver to 3:28 produce 3:28 many different types of substances, proteins, such as fibrinogen, important in 3:35 repair, 3:36 and then it also secreats -- the liver also secreats a protein called C-re 3:41 active protein, 3:42 which is a mediator of inflammation, and it's also used to measure inflammation 3:45 within 3:45 our body. 3:46 The liver also produces a Mandose-binding lectin, which is an important 3:51 component of the complement 3:53 system. 3:54 It activates a certain pathway in the complement system, but we really won't 3:57 talk about that. 3:58 It's just important to know that the liver secreats these substances during an 4:01 invasion 4:01 of a pathogen, infection, inflammatory process, et cetera. 4:05 So what else does an activated macrophage do? 4:08 Well, the cytokines, the macrophage, activated macrophage secreats causes the 4:11 hypothalamus, 4:12 fat, and muscles to increase the body temperature by different means. 4:19 And now you might think to yourself, "Aha, this is why people get fevers when 4:24 they have 4:24 an infection, for example." 4:27 The activated macrophage also secreats cytokines, which targets the bone marrow 4:31 epithelial cells 4:33 to basically produce more neutrophils, causing more neutrophils to come to the 4:38 injured area 4:39 or infiltrated area. 4:41 And most importantly, the activated macrophage secreats cytokines, which target 4:44 the dendritic 4:45 cells. 4:46 Cytokines, TNF alpha, stimulates the dendritic cells to migrate into the lymph 4:52 nodes. 4:52 So the dendritic cells, the antigen-presenting cells, to migrate to the lymph 4:56 node to initiate 4:57 the adaptive immunity, to activate the adaptive immune cells. 5:01 And this is why the dendritic cell is an important connection between the 5:04 innate immune system 5:06 and the adaptive immune system, because it's an antigen-presenting cell, which 5:09 activates 5:10 the adaptive immune system. 5:12 Also a macrophage is also an antigen-presenting cell, and so it can connect the 5:16 innate and 5:17 adaptive immune systems together. 5:18 However, in this case, the tissue dendritic cells play a more important role. 5:23 And so the tissue dendritic cell, when it recognizes a pathogen, it will become 5:27 active 5:27 activated. 5:28 And when the dendritic cell is activated, it will undergo what's called 5:32 licensing, enabling 5:33 it to move into the lymph nodes, to migrate into the lymph nodes. 5:37 So the dendritic cell will phagocytize a pathogen and express the pathogen on a 5:43 MHC molecule, 5:45 begin processing it to express it on an MHC molecule. 5:48 And then once it does this, it will undergo licensing, which basically where 5:53 the dendritic 5:54 cells begin expressing certain protein on the cell surface, proteins, for 5:58 example, CCR7 6:00 here in orange. 6:02 And CCR7 is essentially like a magnet, which has an attraction to chemical 6:08 signals coming 6:09 from the lymph node, chemokines. 6:13 So just to draw again here, we are in the site of inflammation and infection 6:18 here, where 6:19 the pathogen has infiltrated the body. 6:21 Okay, and so this activated dendritic cell, as I mentioned earlier, expresses, 6:27 for example, 6:27 CCR7, which is attracted to a chemokine CCl21, produced by the lymph nodes, 6:35 allowing the 6:36 dendritic cell to move into, to travel through the lymph vessel and travel to 6:42 the lymph node 6:43 because of this attraction between CCR7 and CCl21. 6:52 So here we have the activated dendritic cell with the antigen of the pathogen 6:57 on the MHC 6:58 complex, with the expressed CCR7 on the cell surface, will be attracted to the 7:04 chemokine 7:05 CCl21 and travel to the lymph node through the lymph vessel, as shown here. 7:12 And so this lymph vessel is traveling towards the lymph node with the dendritic 7:16 cell. 7:17 Let's just leave the dendritic cell there for now, and we'll go back to it. 7:21 So what else do we find in this site of infection, site of inflammation? 7:26 So we have possibly infected macrophage, if the macrophage somehow becomes 7:32 infected. 7:33 And so what happens to an infected cell, or an infected macrophage, is that a 7:37 natural 7:37 kill cell will typically come along and kill the infected cell, and through 7:44 apoptosis, 7:45 or some cell destruction. 7:47 And the process in which the natural kill cell kills an infected cell is a bit 7:51 more 7:51 complex, because it includes inhibitory signals and stimulating signals, but it 7:58 'll be for 7:58 another video. 8:00 And also neutrophils will, of course, quickly go inside the area of 8:06 infiltration. 8:07 And let's just say, after some time, many cells become infected around this 8:11 area. 8:12 And so it is important that the adaptive immune cells become activated. 8:16 And so in the next video, what we'll concentrate on is how the dendritic cell 8:19 will travel to 8:20 the lymph node and activate the adaptive immune cells, because it's bringing 8:25 the antigen of 8:26 the pathogen with it. 8:28 So that's for the next video.