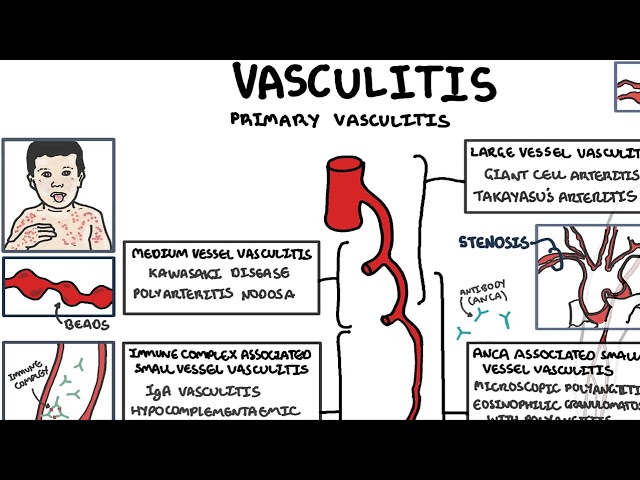
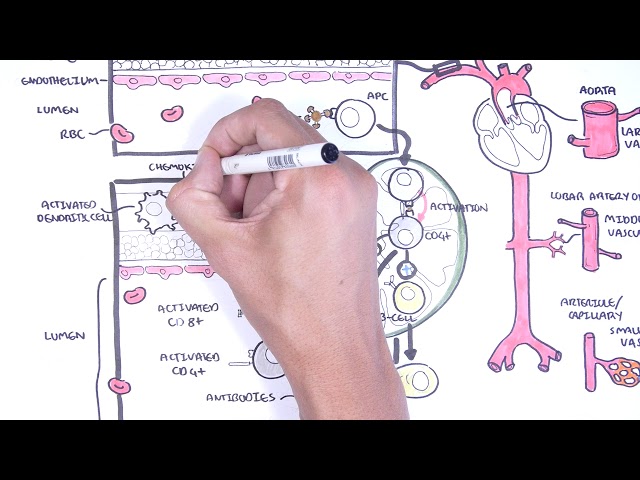
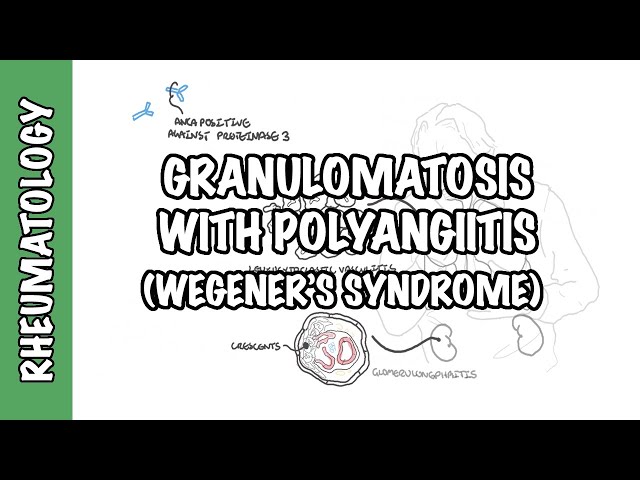
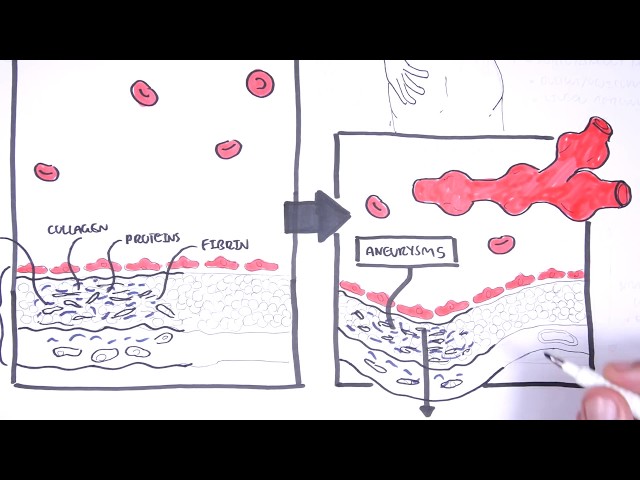
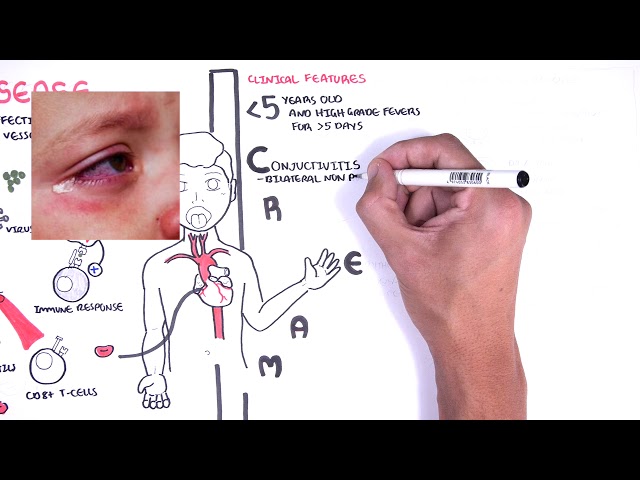
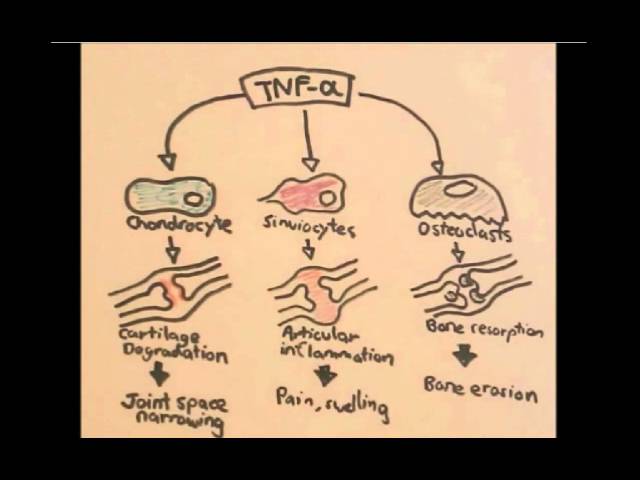
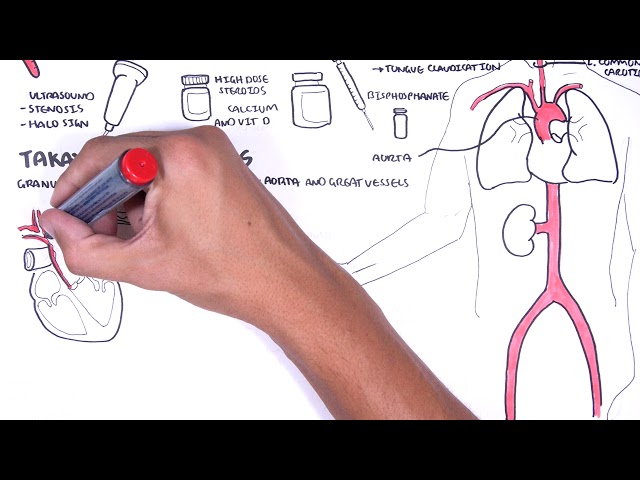
0:00 Hello, in this video, we're going to talk about small vessel vasculitis, 0:06 specifically 0:07 focusing on anchor-associated vasculitis. 0:12 Now, vasculitis is inflammation of the blood vessel, resulting in damaged 0:16 vessels, leading 0:17 to potential complications such as tissue ischemia and even aneurysms. 0:23 Primary vascularities are classified into the size of the blood vessel affected 0:28 . 0:28 Large vessel vasculitis, medium vessel vasculitis, and small vessel vasculitis. 0:33 Small vessel vasculitis typically affects the small arterioles and the capill 0:39 aries. 0:39 The small vessel vasculitis can be further divided into anchor-associated vas 0:45 culitis and 0:46 immune complex mediated vasculitis. 0:52 Anchor-associated vasculitis is so-called this because in the person's blood, 0:56 there 0:56 is presence of anchor, which is an abbreviation to anti-neutrophil cytoplasmic 1:05 antibody. 1:06 Anchor-associated vasculitis usually tends to affect small and also medium- 1:13 sized vessels. 1:15 There are three main types of anchor, microscopic polyangitis, granulomatosis 1:22 with polyangitis, 1:24 recentophilic granulomatosis with polyangitis. 1:30 The pathophysiology of anchor-associated vasculitis involves presence of anchor 1:36 and also granulomatosis. 1:40 Anchor targets certain proteins in the cytoplasmic granules of neutrophils and 1:44 monocytes. 1:45 The neutrophils, for example, contain enzymes, myeloperoxidase and proteinase 3 1:50 in granules. 1:51 Now, what is thought to happen is that during inflammation, cytokines such as T 1:56 NF-alpha and 1:57 interleukin-1 stimulates the translocation of proteinase 3 and myeloperoxidase 2:04 to the 2:04 cell membranes, allowing these enzymes to be exposed. 2:09 Anchor-the actual antibodies are produced by plasma cells through an unknown 2:14 cause, possibly 2:15 infection initially. 2:17 The steps involved would be something like antigen-presenting cells will 2:23 activate the 2:24 naive T cells, which reside in lymphoid tissues such as lymphonoids. 2:29 Now, the naive T cells are actually the T-helper cell and their activation 2:34 relies on interleukin-2. 2:37 The naive T-helper cells will stimulate other T cells, sometimes the T-helper-2 2:44 cells. 2:45 Now, T-helper-2 cells are known to stimulate the humoral immune response, that 2:51 is the antibody 2:53 mediated immune response. 2:54 Therefore, here, the T-helper-2 cells will activate B cells to become plasma 3:01 cells. 3:02 Plasma cells produce ANCA, anti-neutrophil cytoplasmic antibody, and ANCA will 3:09 target 3:10 certain proteins in the cytoplasmic granules of the neutrophils and monocytes 3:16 as I mentioned. 3:17 Now, there are two types of ANCA. 3:20 There are cytoplasmic ANCA and perinuclear ANCA. 3:25 Cytoplasmic ANCA, C ANCA, targets proteinase 3. 3:31 Perinuclear ANCA, P ANCA, mainly targets the enzyme myeloperoxidase. 3:37 Normally, ANCA are unable to bind to these antigens because proteinase 3 and my 3:43 eloperoxidase 3:44 reside in the granules of the neutrophils and monocytes. 3:47 But what is thought to happen is that during inflammation, cytokines, such as T 3:51 -N-of-alpha 3:52 and interleukin-1, stimulates the translocation, basically the expression and 3:57 release of these 3:58 enzymes, proteinase 3 and myeloperoxidase, to the cell membrane, allowing these 4:03 antigens 4:04 to interact with the circulating ANCA. 4:09 Here's a diagram depicting the layers of the blood vessel, the top being the 4:14 endothelium 4:15 lining the inside of the vessel. 4:16 Now, the interaction between ANCA and these enzymes, these antigens, will 4:21 stimulate or 4:22 will cause three main things. 4:25 The first is endothelial attachment of neutrophils through activation of the 4:30 neutrophils, allowing 4:31 infiltration to the vessel layer. 4:34 2. 4:35 The neutrophils will then degranulate, will release reactive oxygen species 4:40 causing damage and 4:42 further inflammation to the surrounding area, to the blood vessels. 4:46 3. 4:47 The neutrophils will also release more pro-inflammatory cytokines promoting the 4:53 inflammatory response. 4:55 Remember, the pathophysiology of ANCA-associated vasculitis involves the 5:00 presence of ANCA, 5:02 the antibodies and also granulomatosis. 5:05 So granulomatosis is mediated by T-helper cells, also known as CD4-T cells. 5:14 Specifically, during flare-ups, there are more T-helper cells than there are 5:19 monocytes. 5:20 T-helper activation relies on cytokines to drive the differentiation process. 5:27 Interleukin-4 encourages T-helper to cell activation and so the humoral immune 5:32 response, 5:33 whereas interleukin-12 and interferon gamma encourages T-helper-1 activation. 5:40 Now, interleukin-12 and interferon gamma is seen in acute flare-ups of ANCA- 5:47 associated 5:48 vasculitis, which means that T-helper cells become T-helper-1 cells. 5:55 T-helper-1 cells function to promote the cell-mediated immune response. 5:59 Now the cell-mediated immune response means activation of monocytes and macroph 6:06 ages. 6:06 Another important cell which does not play as big of a role as CD4-T cells are 6:13 the CD8-T 6:15 cells. 6:16 The CD8-T cells also rely on activation by antigen-presenting cells but also 6:21 rely on 6:22 the T-helper cell activation. 6:25 Now these monocytes, these macrophages and all these other immune cells which 6:30 are activated 6:31 will be recruited to the vessel area to where the inflammation is going on and 6:37 they will 6:37 form the granuloma. 6:40 It is a T-cell-mediated granulomatosis. 6:43 However, keep in mind that in one type of ANCA-associated vasculitis, isynoph 6:49 ils play 6:50 a big role, isynophilic granulomatosis with polyangitis. 6:56 Certain pro-inflammatory cytokines promote granuloma formation. 7:03 Now activation of endothelial cells also play a key role in the pathophysiology 7:09 of ANCA-associated 7:10 vasculitis. 7:12 These nucleotic endothelial cells which are the cells that line the inner part 7:15 of the 7:15 blood vessel express receptors for immune cells to attach onto. 7:21 They also release chemokines such as intulukin-8 and other cytokines which 7:25 encourages immune 7:26 cell infiltration. 7:29 This in turn will cause inflammation of the blood vessel, hence vasculitis. 7:36 The cycle continues and acute flare-up will cause activation of many immune 7:41 cells releasing 7:42 pro-inflammatory cytokines. 7:44 This release of pro-inflammatory cytokines such as intulukin-1 and TNF-alpha 7:49 causes activation 7:50 of neutrophils and expression of the antigens, myeloproxidase and proteinase-3. 7:56 Thus, in summary, ANCA-associated vasculitis pathophysiology involves an 8:03 initial trigger, 8:05 possibly an infection, you have B-cell activation and thus ANCA production the 8:11 antibodies, and 8:12 then you have T-cell mediated granular mitosis as well as possibly ecinophilic 8:17 in certain 8:18 type of ANCA-associated vasculitis, and three, you have activation of endot 8:24 helial cells of 8:25 the vessel, promoting vasculitis. 8:28 It is thus important to suppress the immune system, to slow down and put a halt 8:35 on this 8:36 cycle. 8:37 Treatment of ANCA-associated vasculitis involves an induction where active 8:42 disease is put into 8:44 remission, followed by maintenance. 8:48 Induction involves glucocorticoids and cyclophosphamide, now glucocorticoids 8:54 work in a few ways. 8:56 One way glucocorticoids work is by inhibiting transcription factors involved in 9:01 the production 9:02 synthesis of TNF-alpha and intulukin-1, and this will obviously suppress 9:08 inflammation. 9:09 Glucocorticoids also inhibit transcription factors and gene expression involved 9:13 in the 9:14 production of intulukin-2, thereby suppressing T-cell activity. 9:20 Cyclophosphamide is an alkylating agent known for its role in chemotherapy. 9:25 Unless it works essentially by suppressing the immune system, specifically the 9:29 lymphocytes, 9:30 which are the T-cells and the B-cells. 9:37 Rituximab is a synthesized antibody, a monoclonal antibody, against the surface 9:42 protein CD20 9:43 on B-cells. 9:45 By binding onto CD20, Rituximab mediates B-cell breakdown and so reduces 9:51 antibody production. 9:54 For maintenance, methotrexate and azathiopurine, and most recently, Rituximab 10:02 can be used. 10:04 Now that we have a bit of an idea about the pathophysiology behind ankyososian 10:10 vasculitis, 10:11 we can now learn about the three types of ankyososian vasculitis in more detail 10:17 . 10:18 Polyangitis, granular mitosis with polyangitis, ECNophilic granular mitosis 10:24 with polyangitis.