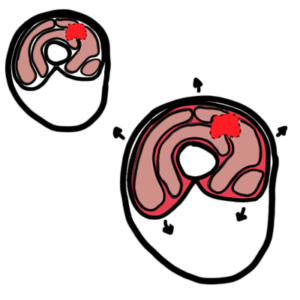
0:00 So let's learn a bit more about the pathophysiology and the mechanism of 0:07 disease. 0:08 When a burn occurs on the skin, it causes changes within the skin that can be 0:14 divided 0:14 into sort of three regions or three zones. 0:19 These zones of a burn were described by Jackson in 1947 and so it is also 0:24 called the Jackson 0:26 model. 0:27 The first zone is the zone of coagulation, then it's the zone of stasis on the 0:32 outside 0:33 and then the furthest part is the zone of hyperimia. 0:38 So the zone of coagulation is essentially the point of maximum damage. 0:44 In this zone, there is irreversible tissue loss due to coagulation of proteins. 0:50 Thus you get coagulative necrosis. 0:53 Running the coagulation zone of necrosis is a zone of stasis. 0:57 Now in this zone, it's essentially characterized by decreased perfusion. 1:02 This ischemic zone may progress to full necrosis unless the ischemia is 1:09 reversed. 1:10 At the very outside is the zone of hyperimia. 1:12 In this outermost zone, tissue perfusion is increased. 1:17 The tissue here is invariably recovered unless there is severe sepsis or 1:22 prolonged hypo perfusion. 1:25 Again the stasis zone is characterized by ischemia and may progress to full nec 1:30 rosis unless the 1:31 ischemia is reversed. 1:34 Therefore, the main aim of burns resuscitation is to increase tissue perfusion 1:40 here and prevent 1:42 any further damage, any damage becoming irreversible. 1:47 So that is a general pathophysiology or mechanism of disease concept of burns. 1:54 When you assess a burn, it is important to know the cause of the burn as we 1:58 have learned 1:58 such as if it's a thermal or radiation burn. 2:02 The other important aspect of a burn assessment is to know the depth of the 2:06 burn. 2:06 To make it super easy, just think of burns as initially being superficial burns 2:12 or deep 2:13 burns. 2:14 So let's zoom into the skin here to look at what happens in a superficial burn 2:18 and what 2:18 happens in a deep burn. 2:20 Let's take a look at a superficial burn first. 2:23 If it's a superficial burn, it will cause damage to the epidermis and the upper 2:28 dermis 2:28 only. 2:29 So like the papillary layer of the dermis. 2:32 Again you have blood vessels here, capillaries. 2:35 Spiritual burns will damage the keratinocytes, which are your cells in the ep 2:40 idermis and 2:41 will also activate an immune response. 2:44 So will activate immune cells around the area such as mass cells and macroph 2:49 ages. 2:49 The damaged keratinocytes, the mass cells and the macrophages will secrete pro- 2:54 inflammatory 2:55 cytokines triggering an immune response. 2:59 The cytokines will stimulate nerve endings around the dermis. 3:03 The sensory nerve endings here can be the ones that detect pain for example and 3:08 pain 3:08 is an important feature of superficial burns. 3:13 Some cytokines will cause increase in vascular permeability. 3:18 The increase in vascular permeability will cause fluid to leak out and may lead 3:23 to interstitial 3:24 edema. 3:28 As the fluid leaks out, it can result in hypertension. 3:33 Remember that the increased in vascular permeability causes fluid to leak out. 3:37 The fluid can actually accumulate in one area causing a blister on the skin 3:43 surface. 3:44 The sensitive blister can rupture and release fluid onto the damaged skin 3:48 surface. 3:49 Thus superficial burns have a moist appearance. 3:54 The cytokines secreted by the cells above will also cause concurrent vasod 4:00 ilation causing 4:00 further hypotension in severe cases. 4:06 The vasodilation contributes to the warmth in the area as well as causing bl 4:11 anching of 4:12 the skin and erythema. 4:16 Blanching means that when you press on the burnt skin surface, blood will 4:20 quickly fill 4:20 it up because of the increase in blood flow to the area. 4:25 The blanching skin is a feature of superficial burns. 4:31 In deep burns, you have more than just damage to the epidermis and upper part 4:36 of the dermis. 4:37 You have damage all the way down, extends all the way to the hypodermis, so it 4:42 's a pretty 4:43 deep burn. 4:46 Deep burns can thus damage blood vessels in the skin. 4:50 Because you have damaged blood vessels, everything will leak out. 4:54 You have no blood supply to the area, so you eventually get this dry non-blanch 5:00 ing surface. 5:01 It is dry and inelastic. 5:04 The non-blanching dryness is an important feature of deep burns. 5:09 Further, deep burns extending to the particular layer of the dermis can destroy 5:15 nociceptus 5:16 and other sensory nerve fibers. 5:19 Initially pain can be detected, but as the sensory nerve fibers are damaged, 5:24 you get 5:24 hypothecia, so you get reduction in sensation. 5:29 Loss of sensation is an important feature of deep burns. 5:33 Obviously, not all your blood supply is damaged or your blood vessels are 5:38 damaged. 5:39 The functional blood vessels will react to the cytokines produced around the 5:44 area. 5:44 The vessels will increase vascular permeability, which will cause fluid to 5:49 shift out causing 5:50 interstitial edema. 5:53 Fluid shifts out from the intravascular space, so the blood vessel, into the 5:58 interstitial 5:59 and this huge amount of fluid coming out of the vessels will result in hypot 6:06 ension, so 6:07 circulatory shock even. 6:10 Hypotension as a result of the shift of fluid occurs more in deep burns rather 6:13 than superficial 6:14 burns.