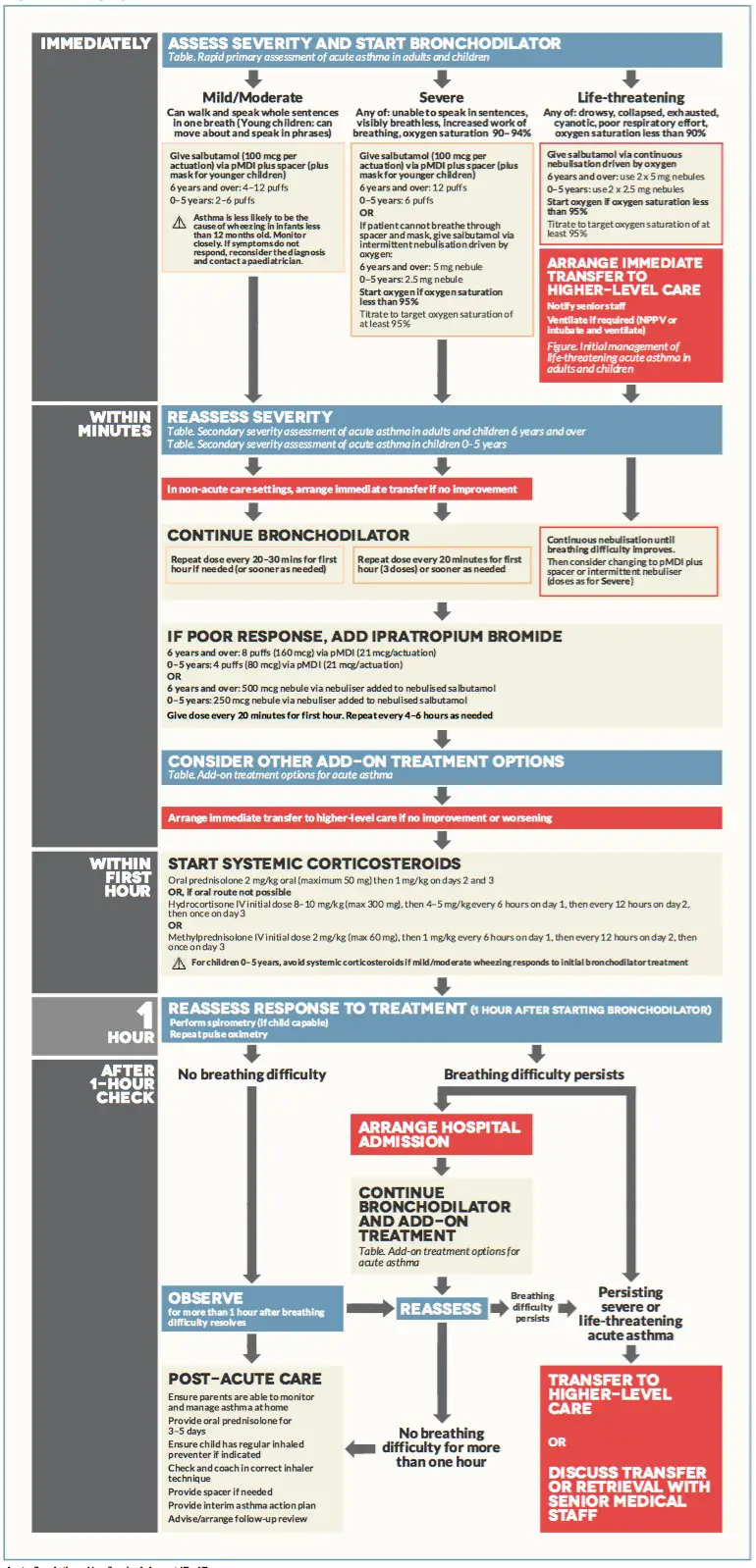
| Remember Assess severity and start bronchodilators! |
Mild-Moderate (maybe admitted to hospital or more likely may improve and go home)
Severe (admitted to hospital)
Life-Threatening (Admitted to hospital possible transferred to a higher level faculty)
| Think Take note if person can talk in whole sentences, phrases, words or can't talk at all! |
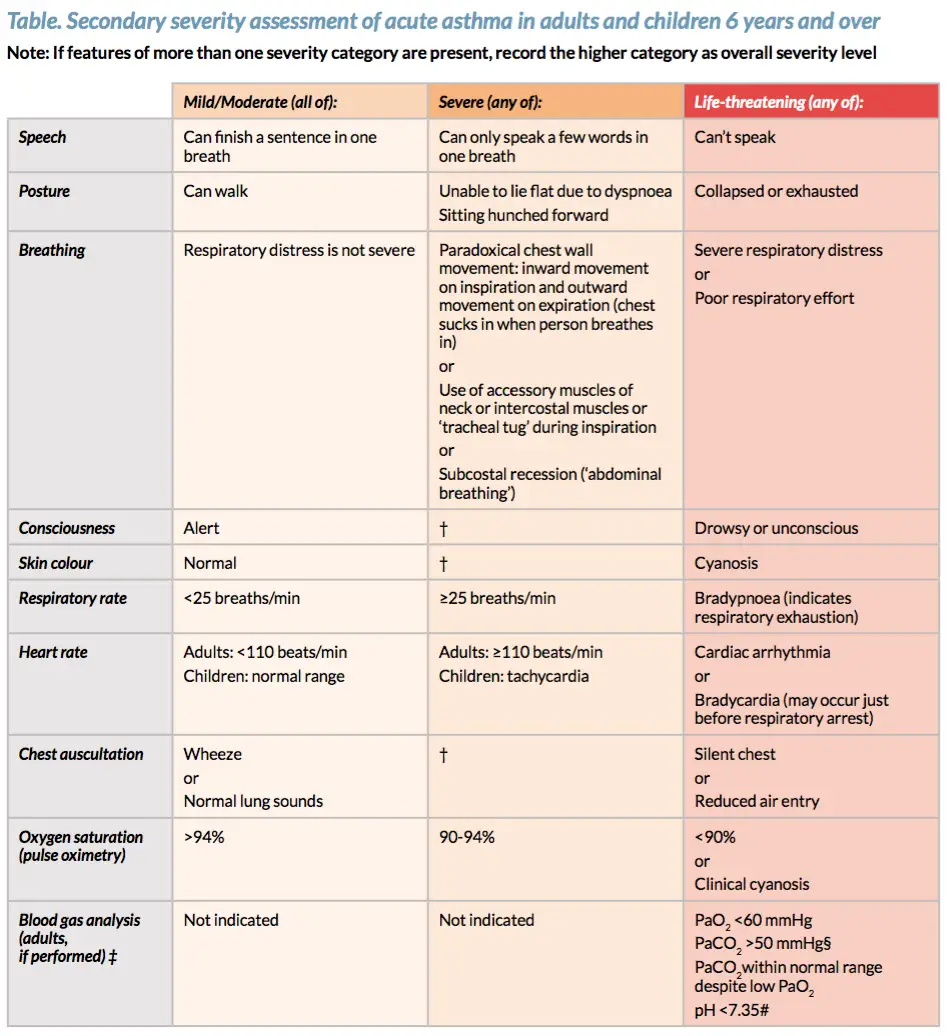
| Remember Assess severity and start bronchodilators! |
Mild (maybe admitted to hospital or more likely may improve and go home)
Management:
| Remember If not responding to any treatment during the 1 hour after bronchodilator, immediate transfer to high level care → move to life-threatening management |
Discharge
Severe asthma defined as:
Management
| Indications for invasive ventilation in asthma |
| Coma |
| Respiratory arrest |
| Exhaustion |
| Deteriorating ABG |
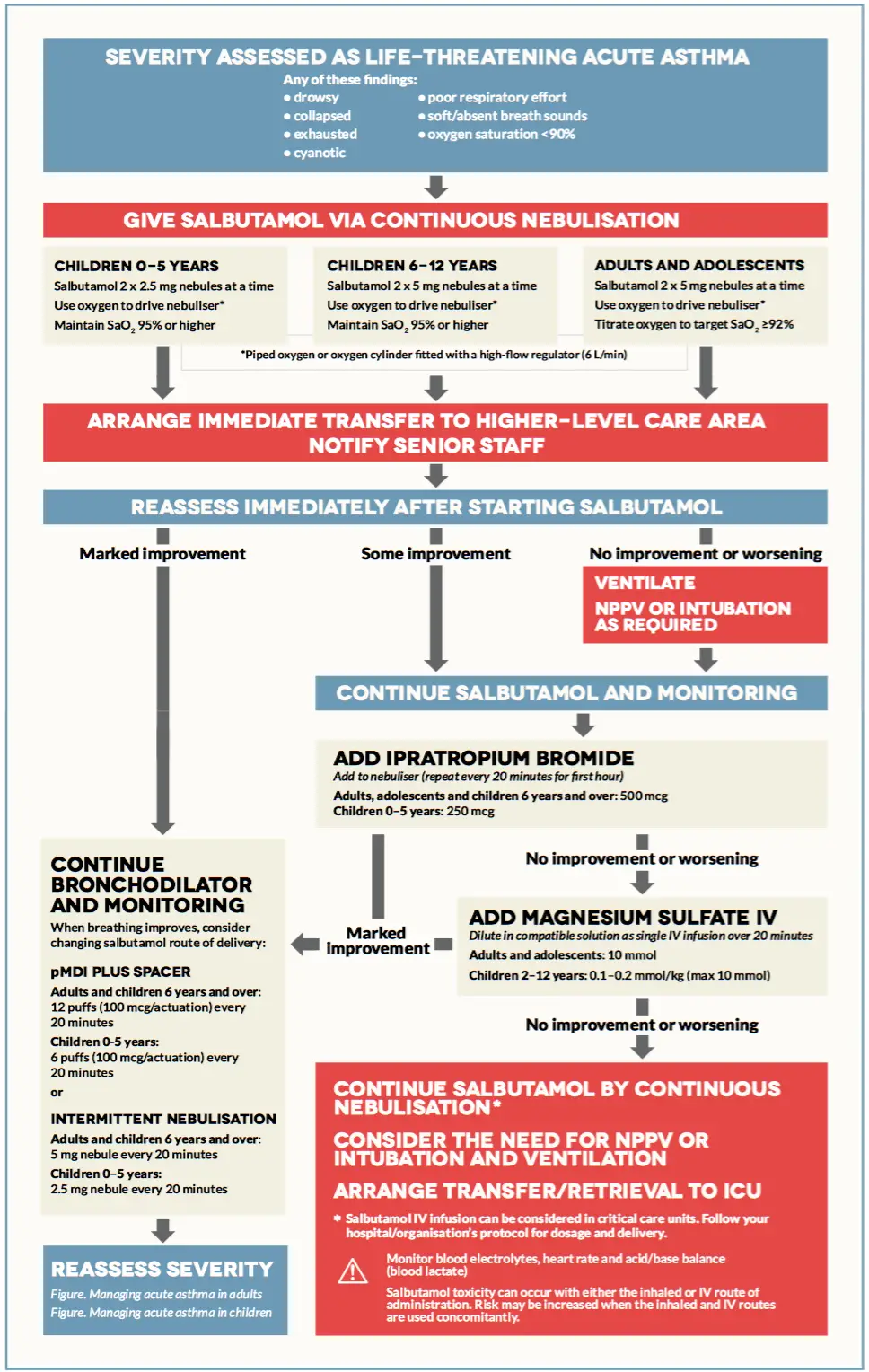
Life-threatening asthma any one of:
| Remember Mneumonic CHEST for life-threatening asthma: Cynosis, Hypotension and Hypoxia (pO2 <90%), Exhaustion, Silent chest, Tachycardia and Threatening PEF < 33% best or predicted (in those >5yrs old) |
Management
| Indications for assisted ventilation in asthma |
| Coma |
| Respiratory arrest |
| Exhaustion |
| Deteriorating ABG |
| Remember Mneumonic O-SHIT-MI for the management of Severe/Life-threatening asthma: Oxygen, Salbutamol, Hydrocortisone (Prednisolone), Ippatropium bromide, Theophylline, Magnesium sulphate, Intubation and ventilation |
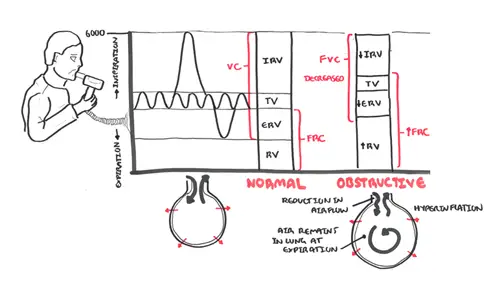
Airway obstruction occurs due to a combination of:
Long-term uncontrolled asthma can lead to air trapping and asthma exacerbations through what is called dynamic hyperinflation.
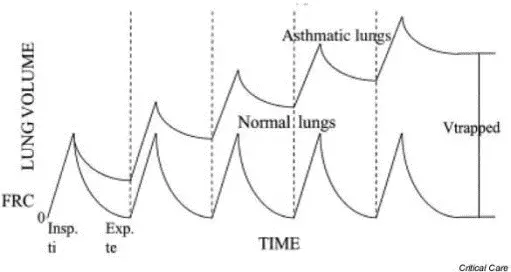
Mild asthma
As asthma gets more severe
Most asthma deaths occur outside hospital and are:
