Overview
Type 1 diabetes is B-cell destruction leading to absolute insulin deficiency. It accounts for 5-10% of all diabetes. Type I diabetes is divided into two types: Immune mediated and idiopathic. The traditional paradigm is of childhood onset with acute symptoms of DKA.
Definition
Diabetes: A group of metabolic diseases in which there are high blood sugar levels over a prolonged period.
Diabetes Mellitus Type I: Autoimmune destruction of beta cells in the pancreas
Diabetes Mellitus Type II: Insulin resistance followed by beta cell atrophy
Gestational Diabetes: diabetes diagnosed during the second half of pregnancy with no prior existing diabetes.
Diagnosis
The age of onset and rate of B-cell destruction is quite variable:
- Rapid in infants and children
- Slow in others (mainly adults) such as occurs in Latent Autoimmune Diabetes of Adulthood (LADA).
This influences clinical presentation and may confuse diagnosis.
Diagnosis
Acute onset of hyperglycaemic symptoms with ketoacidosis:
- Random plasma glucose > 11.1 mmol/L consistent with diagnosis
- HbA1c is not used in diagnosis
Autoimmune markers are not routinely used but can include:
- Glutamic acid decarboxylase (GAD65)
- Insulin (IAA)
- Tyrosine phosphatases (IA-2 & IA-2B)
- ZnT8
Low or undetectable plasma C-peptide level supports the diagnosis.
Latent autoimmune diabetes of adulthood
- A subtype of autoimmune Type 1 diabetes sometimes misdiagnosed as T2D.
- Slowly progressive destruction of Beta cells.
- May appear to respond to oral agents initially.
- Less likely to have other features of metabolic syndrome (central obesity, HT, dyslipidaemia).
- More likely to have history of other autoimmune diseases.
- Starting insulin early may help to preserve beta cell insulin production
Criteria to standardize the definition:
- Age of onset usually > 30y
- Positive titre for at least one T1D autoantibody
- Not treated with insulin within the first 6 months after diagnosis
Treatment
General target
- HbA1c target <7
- BSL 4-6 pre meal and 4-8 post meal
Non-pharmacological methods
- Patient education and pscyhosocial support
- Hypoglcyaemic symptoms and management
- Driving
- Glucose monitoring
- Self glucose monitoring
- Continous glucose monitoring (which measure inersitial glucose)
- Multidisplnary team
- Opthalmologist
- Nephrologist
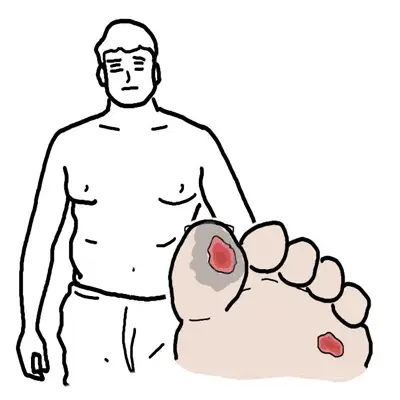
- Podiatrist
Pharmacological treatment
- Insulin (causes weight gain)
- Continous subcutaenous insulin pump therapy
- Non-insulin treatment (all cause weight loss)
- Pramlintide
- Metformin
- GLP-1 receptor agonist
- SGLT2 inhibitors
Surgical treatment
- Pancreas transplantation (curative)
- Islet transplantation
Complications and Prognosis
Complications
- Increased risk of other autoimmune disease
- Autoimmune thyroid disease
- Addison's disease
- Coeliac disease
- Vitiligo
- Diabetic ketoacidosis