Overview
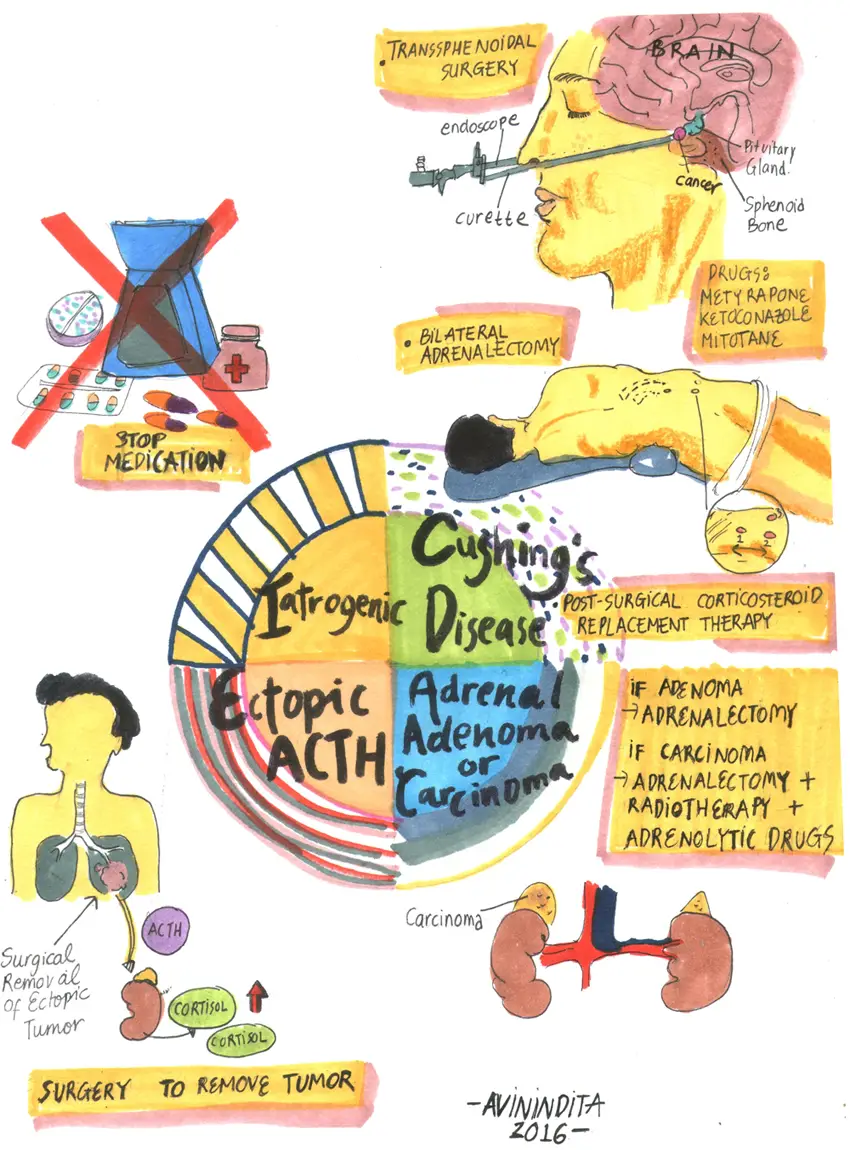
Cushing’s disease is a ACTH dependent syndrome characterised by excess corticosteroid production from the adrenal glands. It is ACTH dependent because it is triggered by an ACTH-secreting pituitary tumour. Cushing’s syndrome is an over arching term to describe hypercortisolaemia dependent of independent of ACTH. Adrenal Cushing’s syndrome is different because it is hypercortisolaemia independent of ACTH.
| Definition Cushing’s syndrome (CS): is a disease complex that results from chronic hypercortisolemia of any cause. The causes may be classified as ACTH dependent and ACTH independent. Cushing’s disease (CD): is hypercortisolemia from an ACTH-secreting pituitary tumor (ACTH Dependent) ACTH-independent Cushing’s syndrome is due to adrenal tumors (benign and malignant) and is responsible for 10–20% cases of Cushing’s syndrome. |
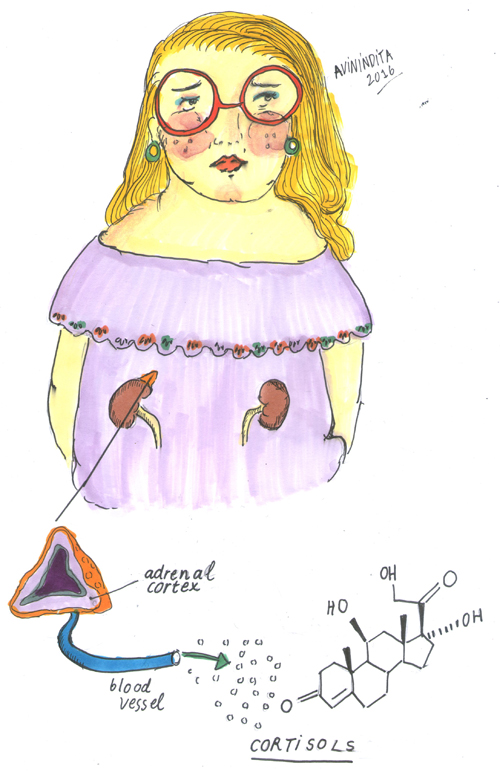
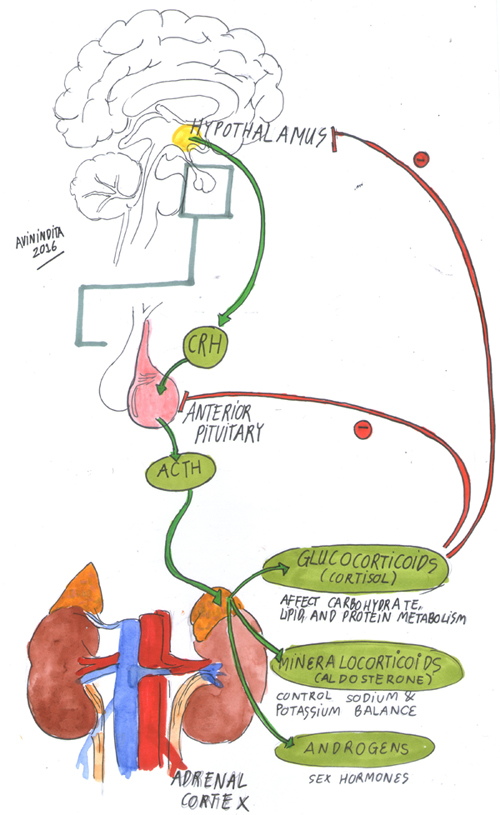
Adrenal Glands Anatomy and Physiology
Anatomy
- The normal adrenal glands weigh 4–5 g.
- The cortex represents 90% of the normal gland and surrounds the medulla.
- The arterial blood supply arises from the renal arteries, aorta, and inferior phrenic artery.
- Venous drainage occurs via the central vein into the inferior vena cava on the right, and into the left renal vein on the left.
- Three layers of the adrenal glands
- Zona fasiculata
- Zona glomerulosa
- Zona Reticularis
Physiology
- Glucocorticoids (zona fasciculata)
- Mineralcorticoids (zona glomerulosa)
- Androgens (zona reticularis and zona fasciculata)
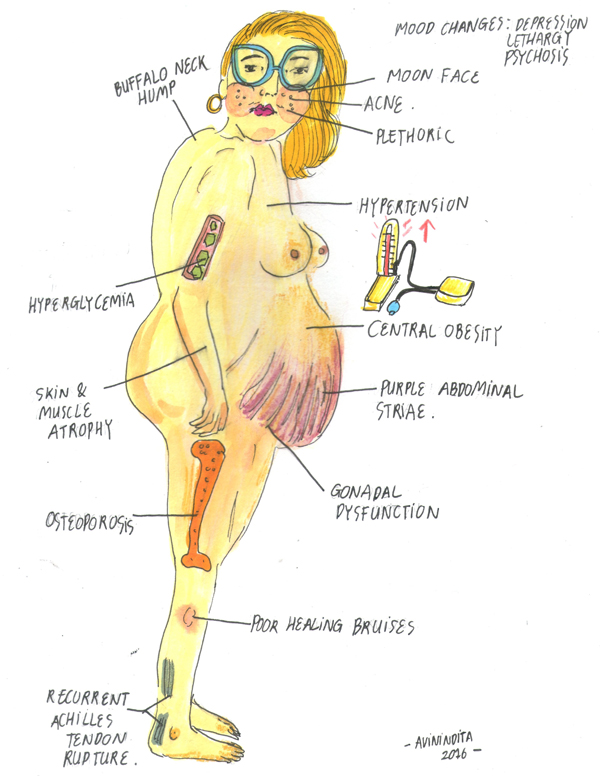
Clinical Manifestation
Diagnosis
Differential Diagnosis and causes of Cushing’s syndrome
ACTH-dependent
- Pituitary adenoma (Cushing’s disease): 70–80%
- Ectopic ACTH syndrome: 10%
- Ectopic CRH secretion: <1%
ACTH-independent
- Adrenal adenoma: 10–20%
- Adrenal carcinoma: <5%
- Nodular (macro or micro) hyperplasia: 1%
- Carney’s complex
- McCune–Albright syndrome
Exogenous Causes
- Iatrogenic etiologies (e.g., oral, inhaled or topical steroids) are the most common cause of CS
- Pseudo-Cushing’s disease
- Glucocorticoid resistance syndrome
Investigations
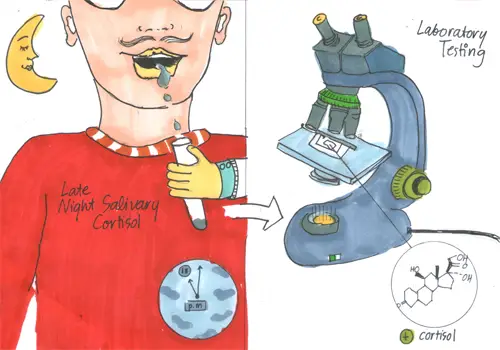
- Screening tests
- 24 hour urinary free cortisol (at least 2 measurements) – Gold Standard
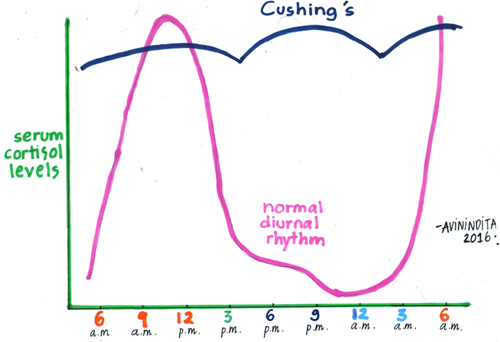
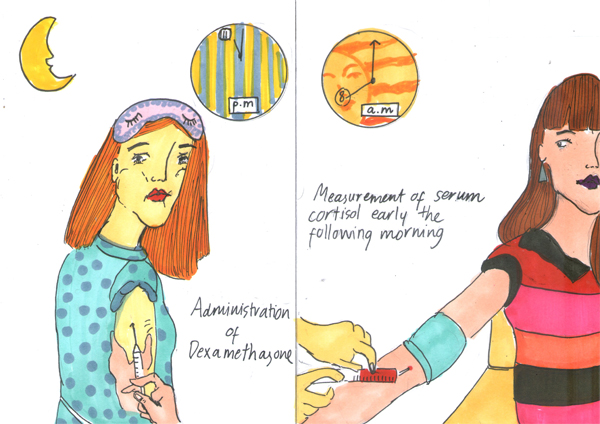
- Overnight Dexamethasone Suppression test – Can be used initially to rule out Cushing’s syndrome and also to assess function of ACTH
- Serum ACTH Levels – differentiate between ACTH dependent and independent
- Pituitary imaging
- MRI – detects 50% of tumours in Cushing’s disease
- CT – hypercortisolaemia from a adrenal source
Aetiology
The majority of endogenous Cushing’s syndrome is due to ACTH-secreting pituitary adenomas (Cushing’s disease).
| Remember Cushing’s Disease is ACTH dependent hypercortisolaemia. Most common cause is pituitary adenoma. |
Treatment
- Transsphenoidal surgery (TSS) – First-line therapy in most Cushing’s disease cases.
- Medical treatment
- Metyrapone
- Ketoconazole
- Mitotane
- Pituitary radiotherapy
- Adrenalectomy In ACTH-dependent Cushing’s, bilateral adrenalectomy is the treatment of last resort
| Pharmacology Metyrapone reduces cortisol production by inhibiting the 11-ß-hydroxylation reaction in the adrenal cortex. Side effects: arrhythmias, hypotension, dehydration, anxiety, confusion, weakness, impairment of consciousness, nausea, vomiting, epigastric pain, and diarrhea. |
Complication and Prognosis
Complications
- Adrenal insufficiency
- Cardiovascular disease
- Hypertension
- Diabetes mellitus
- Osteoporosis
- Nephrolithiasis
- Treatment-related
- Central hypothyroidism
- Growth hormone deficiency
- Adrenal insufficiency
- Hypogonadism
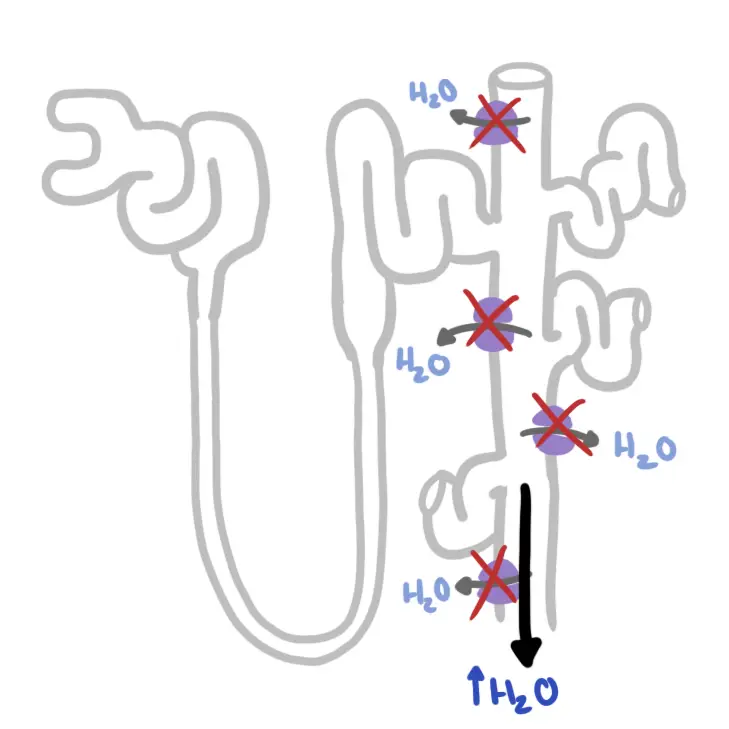
- Diabetes insipidus
- Nelson’s Syndrome
| Nelson Syndrome is a spectrum of symptoms and signs arising from an adrenocorticotropin (ACTH)–secreting pituitary macroadenoma after a therapeutic bilateral adrenalectomy. |
Prognosis
- Without treatment, hypercortisolism persists and in many patients worsens. Untreated -survival rate of 50% at 5 years
- ACTH dependant Cushing’s Syndrome (Cushing’s Disease) – Microadenomas (size <1 cm) have superior outcomes with remission in 65% to 90% of patients. Of these individuals, 5% to 26% have recurrence at 5 years and >10% to 20% have recurrences by 10 years.
Adrenal Insufficiency
Medical Emergency
Adrenal insufficiency results from inadequate adrenocortical function and may be due to destruction of the adrenal cortex (Addison’s disease) or to disordered pituitary and hypothalamic function (secondary causes). In term’s of Cushing’s Disease, adrenal insufficiency can occur after surgery to remove the pituitary tumour. Loss of pituitary ACTH secretion means low adrenal hormones produced resulting in adrenal insufficiency.
Features of secondary adrenal insufficiency include:
- Anorexia and weight loss (>90%)
- Tiredness
- Weakness—generalized, no particular muscle groups
Pigmentation—generalised—skin is paleDizziness and postural hypotensionAbsence of mineralocorticoid deficiency- GI symptoms—nausea and vomiting, abdominal pain, diarrhea
- Arthralgia and myalgia
- Symptomatic hypoglycemia—rare in adults
- Axillary and pubic hair and reduced libido in women
- Associated features of underlying cause, e.g., visual field defects if there is a pituitary tumor
- Other endocrine deficiencies may manifest due to pituitary failure
- Acute onset may occur due to pituitary apoplexy.