This section will mainly focus on Primary Parathyroidism
Overview
Primary Hyperparathyroidism (PHPT) is generalised disorder calcium, phosphate and bone metabolism due to increased secretion of parathyroid hormone normally leading to hypercalcaemia and hypophosphatemia. PHPT may present with recurrent nephrolithiasis, peptic ulcers, mental and muscle changes and less frequently bone resorption. Frequently, routine blood tests will pick up hypercalcaemia asymptomatically.
| Definition Hyperparathyroidism: Abnormally high concentration of parathyroid hormone in the blood, resulting in weakening of the bones through loss of calcium. Primary Hyperparathyroidism: Excessive production of parathyroid hormone due to hyperactivity or growth of the parathyroid gland. Secondary Hyperparathyroidism: Excessive production of parathyroid hormone in response to low serum calcium Tertiary Hyperparathyroidism: Excessive production of parathyroid hormone after a long period of secondary hyperparathyroidism Multiple Endocrine Neoplasia (MEN): hereditary group of disorders that affect the body's network of hormone-producing glands. The main types are MEN1 and MEN2 |
| Side note Hypoparathyroidism causes hypocalcaemia leading to muscle cramps and twitching and can lead to tetany. |
Anatomy and Physiology
Anatomy of the Parathyroid Gland
The parathyroid glands are tan-coloured, bean-shaped structures, about the size of a grain of rice. There are 4 parathyroid gland which lie on the posterior surface of the thyroid gland.
Embryology Parathyroid development begins around the fifth or sixth week of life at the level of the pharynx, with all parathyroids migrating down into the neck.
- The superior parathyroids are derived from the fourth branchial pouches (along with the ultimobranchial bodies, which differentiate into the parafollicular or C-cells, that secrete calcitonin).
- The inferior parathyroids are derived from the third branchial pouches, along with the thymus. The inferior parathyroid sits above the thymus. This close relationship explains why parathyroid tumours may be found within the substance of the thymus and in the mediastinum
Arterial Blood supply
- Inferior thyroid artery ← Thyrocervical trunk ← Subclavian artery
Lymphatic drainage - along with those of the thyroid gland
- Deep cervical lymph nodes
- Paratracheal lymph nodes.
Nerve supply
- Thyroid branches of the cervical sympathetic ganglia - mainly sensory function, detecting stretch within the glands that gives rise to the sensation of pain in some disorders.
Pathology The parathyroid gland are made up of 4 main cells:
- Chief cells - secrete the parathyroid hormone (PTH)
- Oxyphil cells - these have a secretory function, and tend to become more common with age, but their precise role is not clear
- Adipose tissue - these are fat cells which add bulk to the glands and increase with age and obesity
- Fibrovascular stroma - this is fibrous tissue that gives form to the glands containing the capillaries supplying them with blood
Physiology of the Parathyroid Gland
Parathyroid gland main purpose is to synthesise and secrete parathyroid hormone (PTH). The parathyroid hormone does this in response to blood calcium levels.
- ↓Serum Ca2+ → Stimulates Parathyroidgland → Chief cells secrete PTH → ↑PTH aims to ↑Serum Ca2+
The normal range of serum calcium is 2.25-2.65mmol/L
The skeleton contains 98 percent of total body calcium; the remaining 2 percent circulates throughout the body. One half of circulating calcium is free (ionized) calcium, the only form that has physiologic effects. The remainder is bound to albumin, globulin, and other inorganic molecules. Low albumin levels can affect the total serum calcium level. Measuring the corrected calcium is diagnostic for hypercalcaemia.
- Corrected calcium: ~50% of serum calcium is normally bound to proteins (such as albumin) - therefore leaving only a certain amount bioactive and free. In instances of reduced protein, i.e. hypoalbuminemia – there will be more free calcium since it is not bound. Hence corrected calcium levels.
Aetiology
Primary hyperparathyroidism is caused by the inappropriate secretion of PTH, leading to hypercalcaemia. Causes:
- Parathyroid adenomas (85%)
- MEN 1 and MEN 2 (15%)
- Malignancy (<1%)
- External neck irradiation. Lithium therapy, often used to treat patients with bipolar disorder, can lead to the over-stimulation of parathyroid glands (rare)
| Multiple Endocrine Neoplasia (MEN) are a group of familial endocrine diseases that affect multiple endocrine glands. There are two main types: MEN-1 and MEN-2. |
Clinical Manifestation
Usually present asymptomatic 50%
Stones, Bones, Thrones, Abdominal Groans, Psychiatric Overtones
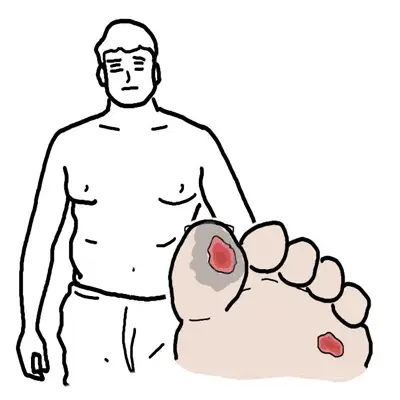
- Stone: nephrolithiasis
- Bones: bone pain, myalgia, muscle cramps
- Thrones: constipation
- Abdominal Groans: abdominal pain
- Psychiatric Overtones: anxiety, depression, memory loss, unsteady gait, poor sleep, parasthesia
| Remember Sudden = more likely malignancy. Chronic = more likely hyperparathyroidism. >3.7 really high = malignancy (parathyroid). |
Diagnosis
More info on Hypercalcaemia here
| DIFFERENT TYPES OF HYPERPARATHYROIDISM | ||
| Condition | Aetiology | Biochemical changes |
| Primary parathyroidism | Adenoma (80%) | ↑PTH,↑Ca, ↓PO4 |
| Secondary parathyroidism | Chronic Kidney Disease, Vitamin D deficiency | ↑PTH, ↓Ca, ↑PO4 |
| Tertiary parathyroidism | Long-term Secondary parathyroidism | ↑PTH, ↑Ca, ↑PO4 |
| Secondary parathyroidism is due to Vitamin D deficiency which together with low Ca2+ stimulates the parathyroid gland (hyperplasia). With an increase in PTH phosphate levels drops but Ca2+ is still low because of no Vitamin D. |
| PTH LEVEL | CAUSE |
| High PTH | Primary or tertiary hyperparathyroidismLithium-induced hyperparathyroidismFamilial Benign Hypocalciuric Hypercalcaemia |
| Low PTH | Malignancy (lung, breast, renal, ovarian, colonic, thyroid carcinoma, lymphoma, multiple myeloma)Elevated Vitamin D (Vitamin D intoxication, HIV, Sarcoidosis) Thyrotoxicosis Paget’s disease |
Investigations
- PTH
- FBC
- EUC
- Vitamin D
- LFTs
- Thyroid Function test
- Urinary calcium
- Multiple Myeloma screening?
Once you have confirmed hyperparathyroidism (i.e. high PTH, high calcium, high urine calcium , low or normal phosphate, high ALP, more likely to be chronic, long standing, hypercalcaemia) then you can consider imaging:
- Bone Mineral Density Scan (DEXA) in primary hyperparathyroidism - Osteoporosis, osteopenia
- Renal imaging (abdo x-ray or U/S) - Nephrocalcinosis
Treatment
The reality of treatment in primary hyperparathyroidism (90% adenoma) is surgical treatment – parathyroidectomy. If asymptomatic – can watch and wait – can give bisphosphonates for bone protection and increase oral fluids to reduce hypercalcaemia and prevent stones – review with serum calcium, PTH measurements and BMD every 6-12 months.
| Indications for Surgical Management |
| <50 |
| Clear cut related symptoms (peptic ulcer, stones, renal impairment, osteopenia) |
| Severe 3.7-4.5mmol serum calcium |
| Consistent follow-up is unlikely |
| Co-existing illness would complicate management |
Complications and Prognosis
Complications
- Post Surgery
- Haematoma
- Hypocalcaemia
- Larygneal nerve injury
- Pneumothorax
- Osteoporosis
- Bone Fractures
- Nephrolithiasis
Prognosis
- Parathyroidectomy has a high cure rate!