Overview
Diabetes Mellitus type II is a progressive disorder defined by deficits in insulin secretion and action (insulin resistance). 1 in 12 people have diabetes (50% do not know they have it). Diabetes type II accounts for over 90% of all diabetes cases. The remaining 10% include type I diabetes. People with type II diabetes are often asymptomatic initially, and may not be recognised for many years. Type II is not usually associated with DKA and insulin is not essential for survival but is often required to achieve adequate glycemic control.
| Definition Diabetes: A group of metabolic diseases in which there are high blood sugar levels over a prolonged period. Diabetes Mellitus Type I: Autoimmune destruction of beta cells in the pancreas Diabetes Mellitus Type II: Insulin resistance followed by beta cell atrophy Gestational Diabetes: diabetes diagnosed during the second half of pregnancy with no prior existing diabetes. |
Anatomy and Physiology
The pancreas sits in the upper abdomen behind the stomach. The pancreas consists of the following parts:
- Head
- Neck
- Body
- Tail
The head is encircled by duodenum and tail in contact with spleen. The pancreas has a poorly developed capsule & therefore adjacent structures (common bile duct, duodenum, splenic vein, transverse colon) are commonly involved in inflammatory process. It is an exocrine and endocrine organ.
Blood Supply
- Pancreatic branches of the splenic artery
- Superior pancreaticoduodenal artery
- Inferior pancreaticoduodenal artery
Venous drainage
- Drains with the splenic vein → Superior Mesenteric → Portal vein
Nerve invervation
- Parasympathetic → Vagus nerve → Stimulates pancreatic juice secretion
- Sympathetic
Lymphatic drainage
- Head and Neck → Pancreticoduodenal nodes →
- Body and Tail → Pancreaticosplenic nodes →
Embryology
- Fusion of the ventral and doral outpounchings of foregut
Exocrine glands bundle up to form the pancreatic acinar which secrete digestive enzymes into the pancreatic duct which makes its way to the ampulla of vater and into the duodenum. The pancreatic duct joins with the common cystic duct. There is the main pancreatic duct and an accessory pancreatic duct which does not join with the common cystic duct so when obstruction occurs due to gallstones, the pancreas is still able to secrete its enzymes into the duodenum. Pancreatic enzymes include:
- Beta-amylase
- Protease
- Lipase
The endocrine cells make up the islets of Langerhan in the pancreas. The Islet of Langerhan make up 2% of the pancreas. There are many endocrine cells:
- Alpha cells → Glucagon
- Beta cells → Insulin
- Delta cells → Somatostatin
The Beta cells produce insulin. The beta cells make up the majority of endocrine cells in the pancreas. Beta cells are stimulated when blood glucose is high. Once insulin is secreted it targets many organs especially the liver to promote glucose storage as glycogen and lipids.
| Watch the video: Fed State |
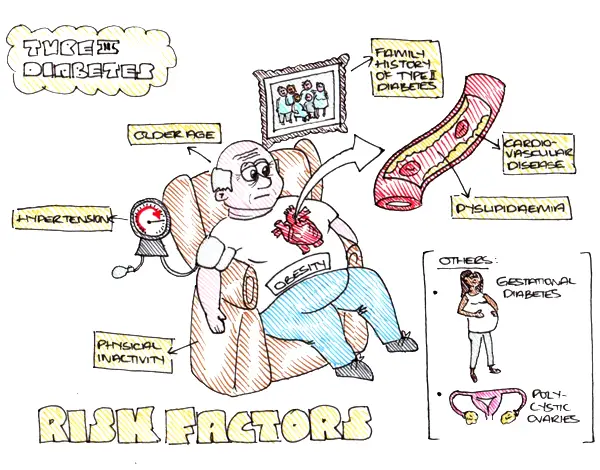
Aetiology and Risk factors
Aetiology
- Genetic predisposition
- Physical inactivity and being overweight contributes to insulin resistance.
Risk Factors
Pathophysiology
| Watch the video: Diabetes Pathophysiology |
| Watch the video: Pathophysiology of Diabetic complications |
Clinical Manifestation
Diabetes in General
- Asymptomatic period
- Infections
- Fatigue
- Blurred vision
- 4Ps
- Paresthesia
- Polydipsia
- Polyuria
- Polyphagia
Diabetic Complications (advanced disease)
Diabetic Retinopathy
- Poor vision
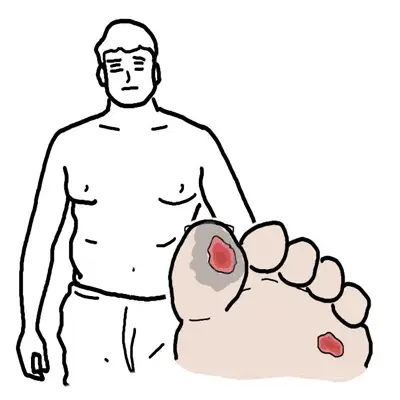
Diabetic Neuropathy
- Peripheral neuropathy
- pain
- loss of sensation
- dysaesthesia
- weakness
- Autonomic neuropathy
- resting tachycardia
- orthostatic hypotension
- erectile dysfunction
- constipation
Diabetic Nephropathy
- Oedema
- Anaemia
- Hypertension
- Uremia
More info on the Long-Term Complications of Diabetes
Investigations
- HbA1c
- Fasting plasma glucose
- Random plasma glucose
- 2-hours post-load glucose
- Lipid profile
- Urine ketones
- Urine albumin
| Side Note Plasma Fructoseamine is an alternative to HbA1c. It correlates with blood glucose levels and has a shorter half. It is a superior marker to HbA1c in pregnancy, in assessing the effect of medication on diabetes, in diseases that affect erythrocyte number (ex. Sickle cell, hemolytic anaemia). |
Diabetes case detection
- Its important to screen for people with risk factors for diabetes. This can be done using venous plasma glucose levels
- In all asymptomatic people whose initial result suggests a diagnosis of diabetes, a confirmatory test must be performed on a separate day.
Diagnosis (7/11 rule)
- Fasting Blood Glucose ≥7.0 mmol/L (on two separate occasions)
- 2 hour postprandial ≥11.0 mmol/L on OGTT- Oral Glucose Tolerance Test (on two separate occasions)
- HbA1c ≥6.5% (48 mmol/mol) (on two separate occasions)
*There is no definitive diagnostic criteria for Diabetes. The criteria varies between countries
| Remember 7/11 rule. 7 at fasting. 11 after eating. |
Diagnosis
Differential Diagnosis for Diabetes Type II
- Diabetes Mellitus type 1
- LADA (latent autoimmune diabetes of the adult)
- Gestational diabetes
- Diseases of the exocrine pancreas (cystic fibrosis, chronic pancreatitis, haemochromotosis)
- Cushing disease
- Glucocorticoid use
- Genetic syndromes (Down's syndrome, Turners syndrome)
| Gestational Diabetes is defined as glucose intolerance resulting in hyperglycemia of variable severity, with onset or first recognition during pregnancy. |
| Diabetes Type I is cause primarily by immune-mediated destruction of the insulin-producing beta-cells. Islet cell antibodies and antibodies to insulin, glutamic acid decarboxylase and the tyrosine phosphatase. This form of diabetes is usually rapid in onset and within five year the person usually has an absolute deficiency in insulin requiring lifelong treatment with insulin, otherwise they risk developing DKA. |
Differential Diagnosis for Diabetic Complications
Differential Diagnosis for Diabetic Retinopathy
- Hypertension
- Retinal vessel occlusion
Differential Diagnosis for Diabetic Neuropathy
- Uraemia
- Vitamin B12 Deficiency
- Hypothyroidism
- Wernicke and Korsakoff
- Cauda equina problems
- Guillian-Barre syndrome
- Charcot-Marie-Tooth disease
| Guillain-Barré syndrome is a disorder in which the body's immune system attacks part of the peripheral nervous system. Its like multiple sclerosis but it effects the peripheral nervous system. |
Differential Diagnosis for Diabetic Nephropathy
- Glomerulonephritis
- Renal artery stenosis
- Renal tract obstruction
- Multiple Myeloma
Treatment
Priorities
- To relieve symptoms of hyperglycemia
- To avoid acute complications of hyperglycemia, such as diabetic ketoacidosis and hyperosmolar nonketotic coma
- To avoid hypoglycemia
- To reduce the risk of long-term end-organ complications
General Management
- Education in self monitoring and emergency
- Monitor HbA1c
- Healthy eating plan
- Exercise program
- Reduction in cardiovascular risk factors (smoking, blood pressure, lipids)
- Pharmacological therapy
- Use of insulin if required
- Screening for complications (more info below)
| Side Note Red blood cells contain haemoglobin HbA. Glucose bind to haemoglobin making glycosylated haemoglobin HbA1c. Once haemoglobin is glycosylated it stays this way until the red blood cell dies. Red blood cells have a turn around of 120days. Therefore monitoring HbA1c can give an estimate of blood glucose control. If the HbA1c is low it means the glucose level has been low for the 120day period - which means diabetes is under control. |
| Indications for Insulin |
| Acute metabolic complications |
| Perioperative in patients undergoing surgery |
| Severe infection |
| Pregnancy and lactation |
| Fasting plasma glucose >300mg/d |
| Failure of oral anti-diabetic agent/contraindication of oral anti-diabetic agents |
Screening for Diabetic Complications
- Diabetic Retinopathy
- Fundoscopy
- Diabetic Neuropathy
- Neuro examination
- Foot check
- Diabetic Nephropathy
- Urinalysis for proteinuria
- Urinary albumin/creatinine ratio
- EUC
- GFR
Complications and Prognosis
Microvascular Complications
- Diabetic Retinopathy
- Diabetic Neuropathy
- Peripheral neuropathy
- Autonomic neuropathy
- Diabetic Nephropathy
Macrovascular Complications
- Coronary Heart Disease
- Cerebrovascular Disease
- Peripheral Vascular Disease
More info on the Long-term Complications of Diabetes
Other complications
- Hypoglycaemia - due to patients treated with insulin or insulin secretagogues
| Remember glucose of 4 hits the floor (hypoglycemic). |
- Alcohol associated hypoglycaemia - alcohol impairs the body's ability to provide glucose and restore low glucose concentrations towards normal.
- Diabetic Ketoacidosis - occurs more often in Diabetes type I and is characterised by hyperglycamiea, polyuria, polydipsia, hyperventilation and dehydration (can occur with type II)
- Hyperosmolar Hyperglycemia - Occurs primarily in type II diabetes and is characterised by marked hyperglyceamic and dehydration without ketoacidosis. It may present as coma in severe cases and can be precipitated by sepsis. Venous thromboemoblism is a common complication of hyperosmolar states and heparin should be used prophylactically.
- Lactic Acidosis - occurs especially if patients with diabetes have renal impairment or they are in a hypoxic state. Most commonly, lactic acidosis occurs in the setting of tissue hypoxia secondary to shock and hypotension. Lactic acidosis can also be caused by Metformin
- Diabetic cardiomyopathy
- Diabetic musculoskeletal complications - cheirarthropathy, carpal tunnel syndrome and frozen shoulder
- Peridontal disease
Prognosis
- Adults with Type II diabetes are twice as likely to die from stroke or MI
- Diabetes is the most common cause of Chronic Kidney Disease worldwide
Type I vs Type II Diabetes
| DIFFERENCES BETWEEN TYPE I AND TYPE II | ||
| Type I | Type II | |
| Epidemiology | Often starts before puberty | Older patients |
| Morphology | Usually lean | Usually overweight |
| Genetics | HLA D3 and D4 | No HLA association |
| Cause | Autoimmune β cell destruction | Insulin resistance/β cell dysfunction |
| Presentation | Polydipsia, polyuria, weight loss, ketosis (can present with DKA) | Asymptomatic. Complications associated with diabetes |
| Complications | DKA | HHS |