Overview Addison's disease is a disease characterised by adrenal insufficiency. Adrenal insufficiency results in a decrease of the adrenal gland hormones: mineralocorticoids, glucocorticoids and to an extent androgens. There are many causes of addison's disease. The most common cause in the developed world is autoimmune (approximately 70% cases). Signs and symptoms of adrenal sufficiency don't really occur until 90% of adrenal function is lost.
| Definitions Adrenal insufficiency: Adrenal insufficiency results from inadequate adrenocortical function and may be due to destruction of the adrenal cortex (primary or Addison’s disease) or to disordered pituitary and hypothalamic function (secondary). Addison's Disease: Primary adrenal sufficiency independent of hypothalamic, pituitary dysfunction Cushing's Disease: Hypercortisolemia from an ACTH-secreting pituitary tumor (ACTH Dependent) |
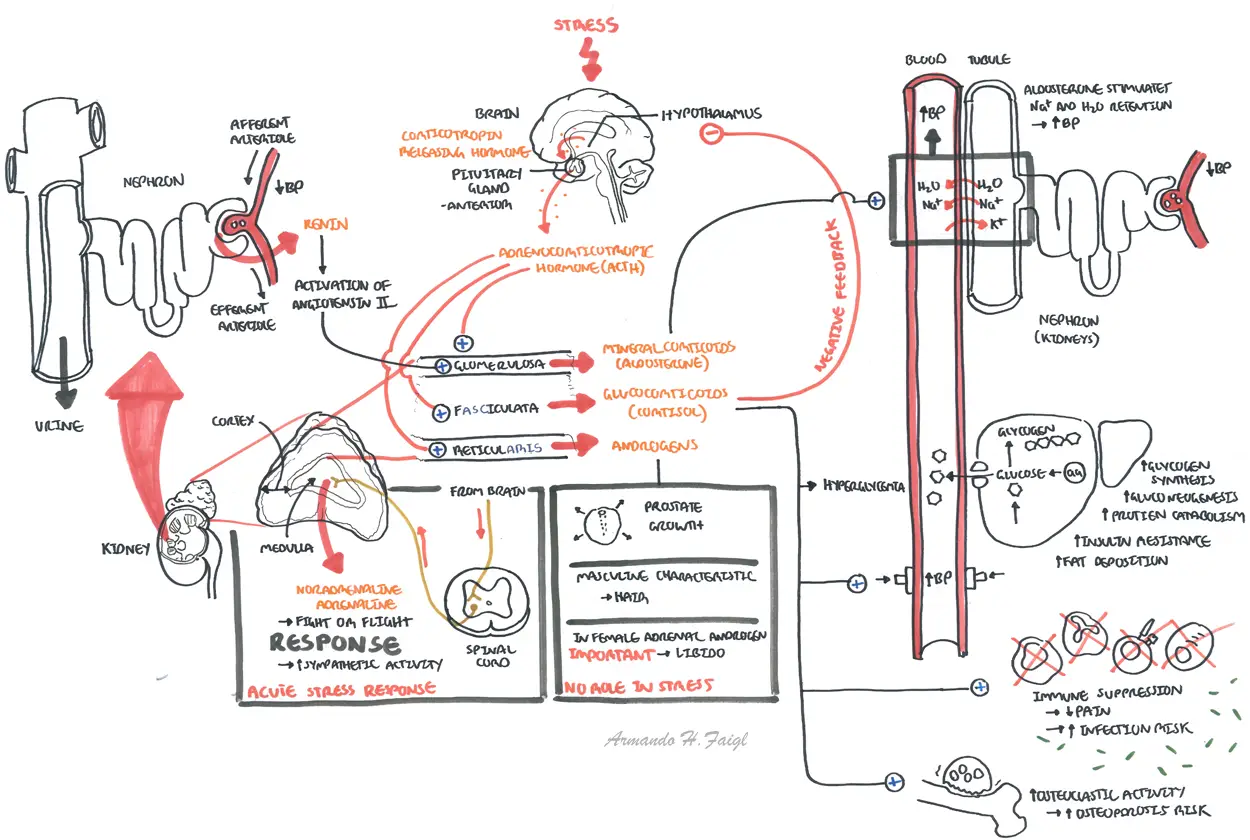
Anatomy
Physiology
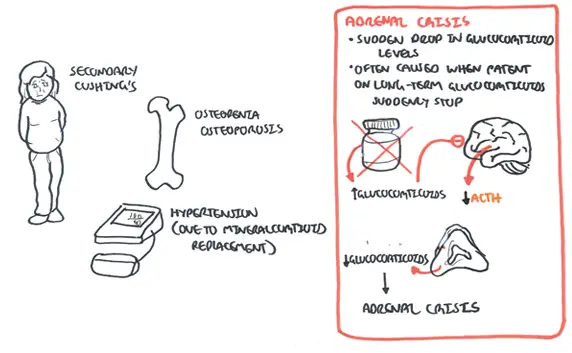
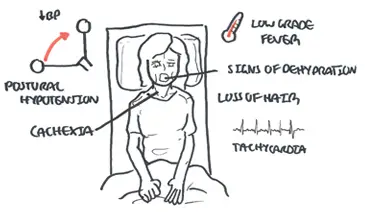
Acute
| Think Acute Adrenal insufficiency (Adrenal Crisis) is commonly caused when patients who are on long term glucocorticoids suddenly stop or do not increase dosage during febrile illness. |
General presentation (Chronic)
Clinical Examination
| Schmidt syndrome Addison's Disease and Autoimmune hypothyroidism |
| Carpenter Syndrome Addison's Disease, Autoimmune hypothyroidism and/or Type 1 diabetes mellitus |
| Think In Secondary Adrenal Insufficiency there is ↓Serum Cortisol and ↓ACTH |

There are many causes of Addison's Disease
Adrenal gland destruction or dysfunction occurs from a disease process that usually involves all three zones of the adrenal cortex, resulting in inadequate glucocorticoid, mineralocorticoid, and androgen secretion. Autoimmunity is the main etiologic factor.
The manifestations of insufficiency do not usually appear until at least 90% of the gland has been destroyed and are usually gradual in onset, with partial adrenal insufficiency leading to an impaired cortisol response to stress, and the features of complete insufficiency occurring later.
Acute adrenal insufficiency may occur in the context of acute septicemia (e.g., meningococcal or hemorrhage).

Mineralocorticoid deficiency leads to reduced sodium retention and hypotension with ↓ intravascular volume, in addition to hyperkalemia due to ↓ renal potassium and hydrogen ion excretion.
Androgen deficiency presents in women with reduced axillary and pubic hair and reduced libido. (Testicular production of androgens is more important in men.)
Lack of cortisol negative feedback increases CRH and ACTH secretion. An increase in other POMC-related peptides leads to skin pigmentation and other mucous membranes.

| Side note Dehydroepiandrosterone (DHEA) is an abundant circulating adrenal androgen with a production rate of 25–50 mg/day. Its levels undergo a progressive decline with ↑ age, and there has been interest in its physiological role. |
| Side note Patient education is the key to successful management. Must be taught never to miss a dose, encouraged to wear a Medic Alert bracelet and every patient should know how to double the dose of glucocorticoid during febrile illness and to get medical attention if unable to take the tablets because of vomiting. |