Author
Megan Miner
Armando Faigl
Overview
Pertussis, also known as “whooping cough”, is a contagious, acute respiratory infection caused by the bacterium Bordetella pertussis. In babies, the infection can sometimes lead to pneumonia and occasionally brain damage and can even be life threatening. Older children and adults can get whooping cough and can spread it to others, including babies. Pertussis causes its severe symptoms via the release of deleterious proteins such as; filamentous hemagglutinin, pertactin, agglutinin, tracheal cytotoxin, pertussis toxin, and adenylate cyclase toxin.
| Triad: afebrile respiratory infection, a whooping cough (with increasing frequency and severity) and coryza |
| Definition Bordetella pertussis: Bacterium that causes an acute respiratory infection which results in a severe “whooping” cough as a consequence of the release of noxious proteins as described above. Bordetella parapertussis: Bacterium that causes pertussis-like-illness without the release of pertussis toxin. A “whooping” cough may or may not be present. Filamentous hemagglutinin (FHA): Protein expressed and secreted by Bordetella pertussis in order to anchor to cilia and attach to host immune cells (macrophages). Pertactin: Protein used by the bacterium in order to anchor to cilia. Agglutinin: Protein used by the bacterium in order to anchor to cilia Tracheal cytotoxin: Paralyzes and kills cilia, allowing the bacterium and mucus to stay “stuck” in the respiratory tract [3]. This elicits a cough reflex. Pertussis toxin: Helps anchor Bordetella pertussis to respiratory epithelium and triggers an increased T cell production. Also makes the respiratory system more responsive to histamine [3] which causes swelling to the airway and the classic “whooping cough”. Adenylate cyclase toxin: Prevents phagocytes from reaching the infection and induces apoptosis in such cells. |
Aetiology and Risk Factors
Aetiology
Bacterium Bordetella pertussis which is easily spread via aerosolized droplets (cough/sneeze etc), especially during the Catarrhal phase.
Bordetella Pertussis is a gram negative coccobacilli.
Risk Factors
- Lack of immunization (regardless of age)
- Immunosuppressed
- Infants under the age of one
- Teenagers, adults, and geriatrics (as the vaccine wears off)
Pathophysiology
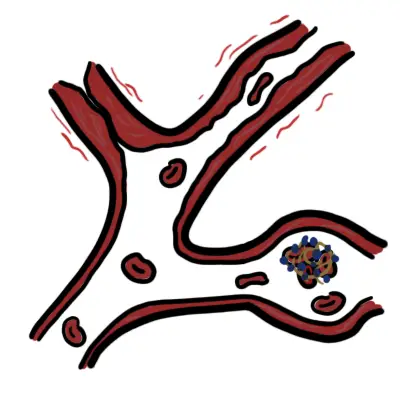
Anchoring virulent factors
- Allow Bordetella pertussis to anchor to epithelia in the respiratory tract
- These include: Filamentous hemagglutinin, pertactin, and agglutinin
Pathogenic virulent factors
- Tracheal Cytotoxin damages, paralyzes, and kills cilia in the airway.
- Pertussis Toxin allows bacteria to attach to surface epithelium of the lungs. It also increases sensitivity of the respiratory tract to histamine which results in edema -> difficulty breathing and also produces the classic “whooping” sound
- Adenylate Cyclase Toxin (CyaA) inhibits the activation and migration of phagocytes to the infected tissues, thus allowing the bacterium to evade the immune system
Clinical Manifestation
Incubation (disease develops in 1-2 weeks)
- asymptomatic
- May have mild cold symptoms
Following incubation there are three stages of the illness. Please note adolescents and adults often don’t present with the classic pertussis syndrome below seen in young children.
Catarrhal Phase (occurs after incubation and lasts roughly 1-2 weeks)
It is best to diagnose pertussis during this phase to reduce mortality and prevent severe damage
- Low-grade fever
- Mild cough
- Nasal congestion
- Highly contagious phase
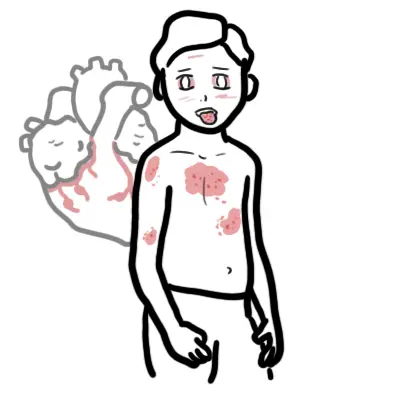
Paroxysmal Phase (occurs after Catarrhal phase and lasts roughly 1-6 weeks)
- “Whooping” cough (due to a swollen glottis)
- Can result in petechiae, vomiting, or a collapsed lung
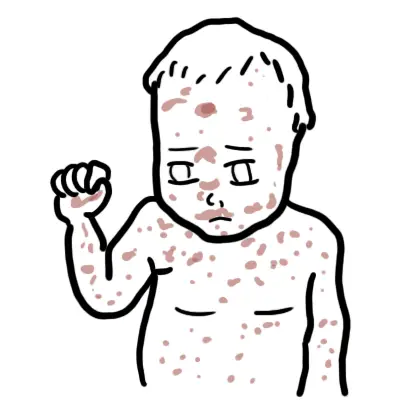
- In infants this can cause
- Hypoxia/cyanosis
- Which can result in seizures, encephalopathy, pneumonia, and death
- Apnea
- Apparent life-threatening event (ALTE)
- Hypoxia/cyanosis
Convalescent Phase (occurs after Paroxysmal phase and lasts roughly 2-3 weeks)
- May still have a mild cough (no longer “whooping” sound)
Diagnosis
- Viral/bacterial respiratory infection
- Bronchiolitis
- Pneumonia
- Tuberculosis
- Common cold
- Influenza
- Cystic fibrosis
- Asthma
- Croup
- Bronchitis
- Respiratory syncytial virus (RSV)
Investigations
- Nasopharynx swab – bacterial growth in culture
- Polymerase chain reaction (PCR) – Identify DNA
- Fluorescent antibody technique – antigen recognition
- Pertussis serology – (late-stage diagnosis), antibody titer
| Remember Culture of nasopharyngeal secretions is considered gold standard for diagnosing pertussis. |
Classification of Genus Bordetella
- Genus Bordetella (most common)
- Contains both the B pertussis and B parapertussis species
- Responsible for causing pertussis in humans
- B bronchiseptica (less common)
- Can cause respiratory illness in humans and other animals
- B avium and B hinzii (rare)
- Rarely cause respiratory disease in humans
Treatment
| Remember pertussis is contagious do not go near babies or pregnant women. |
- Antibiotics – Macrolides
- most useful during the Catarrhal phase or initial Paroxysm phase.
- erythromycin, clarithromycin, and azithromycin (typically used if the patient is older than one month).
- Trimethoprim with sulfamethoxazole can be used as an alternative to macrolides
- For those in close contact with an infected individual, antibiotic treatment is recommended.
- It is recommended that pregnant women be vaccinated in their third trimester
- Vaccination if eligible – tetanus, diphtheria, and pertussis (Tdap) vaccine.
| Side note Treatment with macrolides in infants less than 1 month old should be used with caution due to the association with the development of infantile hypertrophic pyloric stenosis. |
Complications and Prognosis
Complications in Infants and Children
- Apnea
- Pneumonia
- Seizures
- Death
- Encephalopathy
- Dehydration
- Hernias
- Epistaxis
- Pneumothorax
Complications in Adolescents and Adults
- Urinary incontinence
- Syncope
- Dehydration
- Seizures
- Pneumothorax
- Encephalopathy
Prognosis
Those diagnosed with pertussis that are over the age of three months are typically expected to make a full recovery. Those under the age of three months may be associated with more severe symptoms, however mortality rates are less than 3%.
Prognosis is generally grimmer for those that are at-risk (unvaccinated, immunocompromised, or infant/elderly populations).








Discussion