Diabetic Ketoacidosis
| Definition Ketoacidosis: A condition resulting from deficient insulin availability, leading to lipid oxidation and metabolism rather than glucose metabolism. The insulin absence results in free fatty acid (FFA) released from adipose tissue and in unregulated hepatic FFA oxidation and ketogenesis. Type I Diabetes: Autoimmune disease where there is attack of beta cells of the pancreas leading to insulin deficiency and a requirement for exogenous insulin to prevent ketoacidosis. Type II Diabetes: It usually consists of tissue-level insulin resistance (although exogenous insulin is often required) and rarely leads to ketoacidosis. Kussmaul breathing: Deep, rapid respirations associated with acidosis. |
Overview
Diabetic Ketoacidosis may be the presenting feature in a patient not previously recognised as having diabetes. In a patient with known diabetes, it may be precipitated by omitting insulin doses, or by the insulin. Diabetic ketoacidosis has a mortality rate of 8- to 50% in the elderly.
Summary
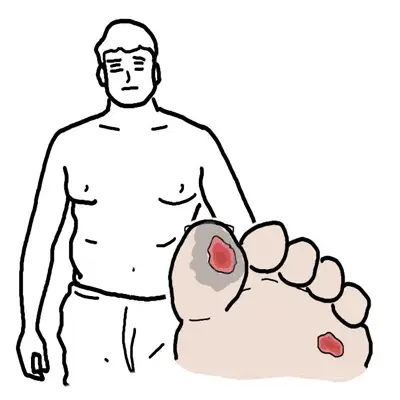
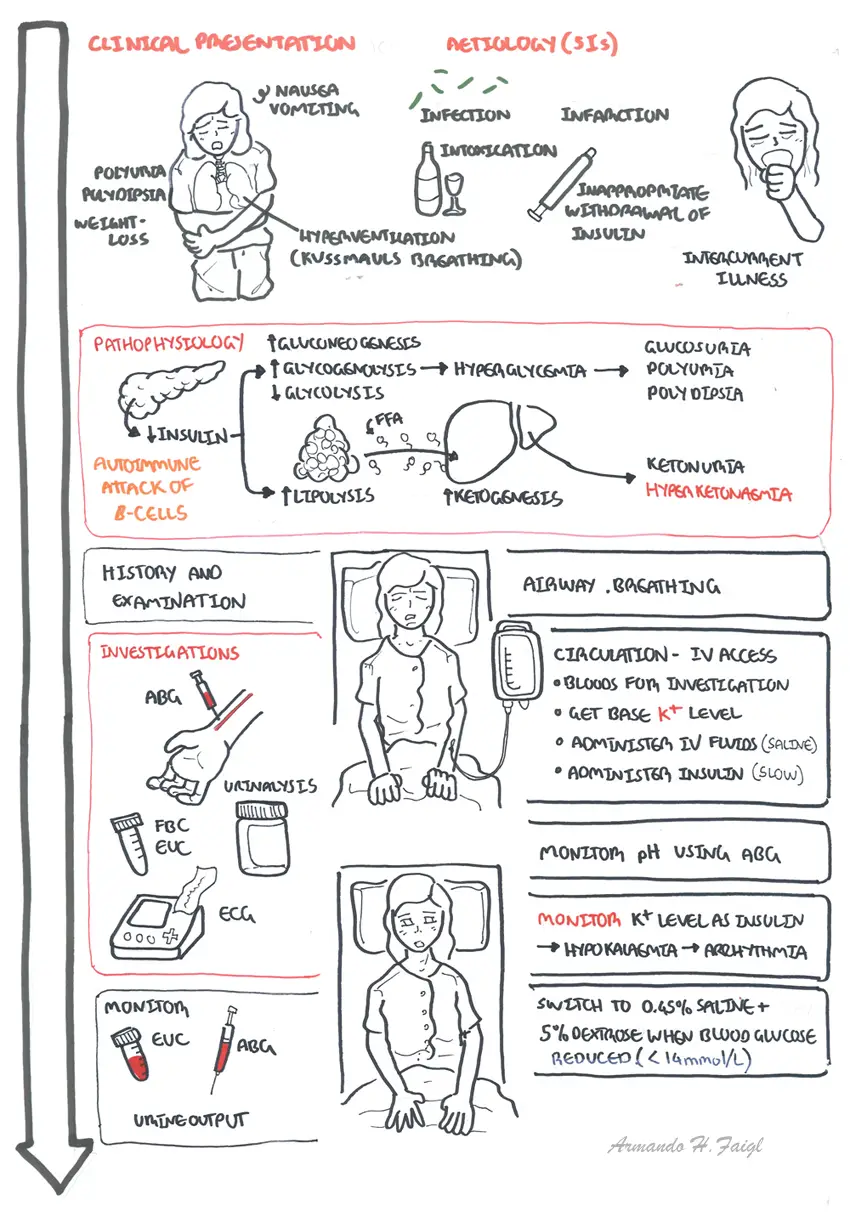
Clinical Presentation
- Signs of dehydration
- polyuria
- polydypsia
- weight loss
- GI symptoms
- Hyperventilation (↑Respiratory Rate - Kussmaul breathing)
- True coma - 10% of cases)
| Side Note Kussmaul breathing is air hunger, rapid deep breathing a sign of metabolic acidosis. This is different to Kusmaul’s sign looks at JVP relationship with breathing. |
Aetiology (5I's) + Initial Diagnosis
- Infection
- Infarction
- Insufficient insulin
- Intercurrent illness
- Inappropriate withdrawal of Insulin
- Initial Diagnosis
| Remember Precipitating factors of DKA 5 I's: Infection Ischemia Infarction Intoxication Insulin missed |
Investigations
- Bloods - EUC, Glucose, bicarbonate (HCO3 - < 12 mmol/L indicates severe acidosis)
- ABG - Assess severity of acidosis
- Urine - Ketones, Glucose
- ECG - Hypokalaemia - arrythmias
- Troponin - in older patients as MI could be a trigger
- Infection screen - FBC, Blood and urine culture, CRP, CXR. Although leukocytosis invariably occurs, this represents a stress response and does not necessarily indicate infection
| Think Check ABG, EUC and glucose every 4hours. Monitor ECG for hypokalaemia/hyperkalaemia. Monitor IV fluid, insulin, glucose and K+ should all be run in separate lines. |
Differential Diagnosis - high blood glucose and coma
- Head injury
- Alcohol
- Drug overdose
Diagnosis of DKA
- Hyperglycemia (>11.1mmol/L)
- Metabolic acidosis (pH <7.3 or <HCO3-)
- Severity is assessed this way
- Hyperketonemia
- Ketonuria
| Side Effects Different types ketones produced include B-Hydroxymutyrate, acetatoacetate and acetone |
Management
The main aim in treating DKA is to progressively improve blood pH and clear the body of excessive ketones by aggressive fluid replacement and insulin therapy.
- Assess Airway, Breathing, Circulation
- IV Fluids - Normal Saline 0.9% NaCL (switch to 5% dextrose with 0.45% NaCl when serum glucose reaches ~15)
- Insulin - Insulin infusion until pH stabilizes
- Potassium - Administration of Insulin can cause hypokalemia, potassium levels should be checked prior to insulin administration
- ABG assessment - assess pH and need for bicarbonate
- Monitoring
- Check ABG, EUC every 4hours.
- Check Urine Glucose and Ketone 4hourly
- Check Blood glucose hourly.
- Monitor ECG for hypokalaemia/hyperkalaemia
- Monitor GCS regularly
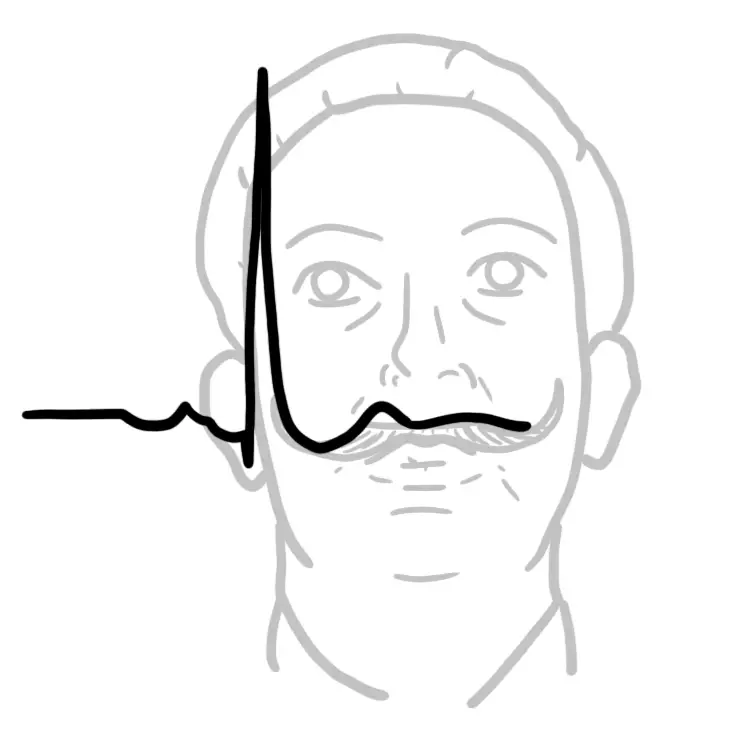
| Remember Hypokalaemia ECG changes include flat/inverted T-wave, ST Depression and widened QRS |
| Glasgow Coma Scale | ||
| Behaviours | Response | Score |
| Eye response (score 1-4) | Spontaneously To Speech To Pain No response |
4 3 2 1 |
| Verbal response (score 1-5) | Orientated good Confused Inappropriate words Incomprehensible sounds No response |
5 4 3 2 1 |
| Motor response (score 1-6) | Obeys command Moves to localised pain Withdrawal from pain Decorticate Decerebrate No response |
6 5 4 3 2 1 |
| Score | Best response Coma Unresponsive (Lowest possible) |
15 <8 3 |
Complications of DKA
- Cerebral oedema
- May be caused by very rapid reduction of blood glucose, use of hypotonic fluids and/or bicarbonate
- High mortality
- Treat with mannitol, oxygen Acute respiratory distress syndrome
- Thromboembolism
- Disseminated intravascular coagulation (rare)
- Acute circulatory failure
Hyperosmolar Hyperglycaemia
| Definition Hyperosmolar Hyperglyaecmic State is a complication of type 2 diabetes. It involves extremely high blood sugar (glucose) levels without the presence of ketones. Type I Diabetes: Is caused by a severe endogenous insulin deficiency and a requirement for exogenous insulin to prevent ketoacidosis. Type II Diabetes: It usually consists of tissue-level insulin resistance (although exogenous insulin is often required) and can lead to HHS, rarely leads to ketoacidosis. |
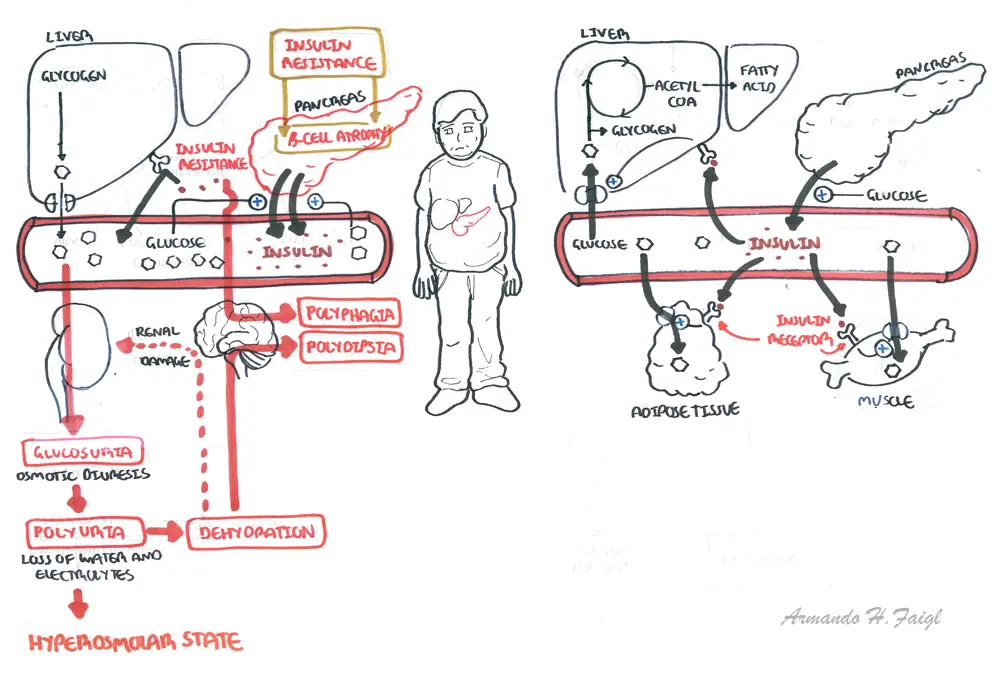
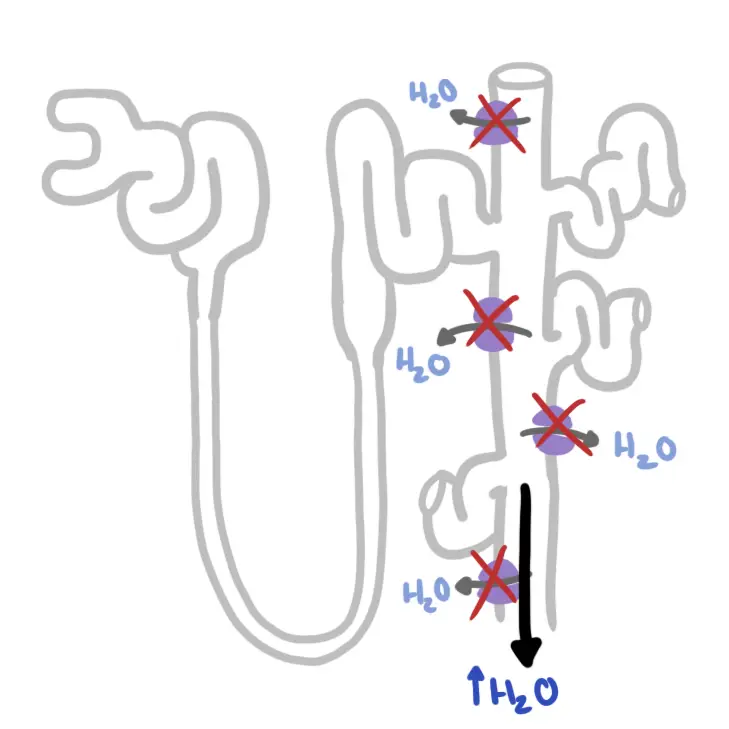
Pathophysiology of Diabetes Type II and Hyperosmolar state
Overview
Hyperosmolar Hyperglycaemia (HOH) state occurring primarily in type 2 diabetes and is characterised by marked hyperglycaemia and dehydration without ketoacidosis. The disturbance in consciousness in patients varies from drowsy to comatose. HOH is a more sinister complication than ketoacidosis with a mortality rate as high as 50%.
Diagnosis - biochemical
- Hyperglycemia
- Serum osmolality is high (>350 mmol/kg)
- No acidosis
- No ketonuria + on urine dip testing can occur with starvation and vomiting.
Serum osmolality (in mosmol/kg) can be calculated if not available from the laboratory using the following equation:
- Osmolality = 2(sodium + potassium) + glucose + urea
Pathophysiology
This condition results from a combination of insulin deficiency and coun- terregulatory hormone excess. The insulin present stops ketone produc- tion but in insufficient quantities to prevent worsening hyperglycemia.
Management
Same as DKA, but with a few exception because patients are usually older.
- IV Fluids - Normal Saline 0.45% NaCL (switch to 5% dextrose with 0.45% NaCl when serum glucose reaches ~15)
- Insulin - Slow Insulin infusion until pH stabilizes
- Potassium - Administration of Insulin can cause hypokalemia, potassium levels should be checked.
- Antibiotics - if infection
- ABG assessment - assess pH and need for bicarbonate
Complication
- Venous thromboembolism
Hypoglycaemia
Coming soon...