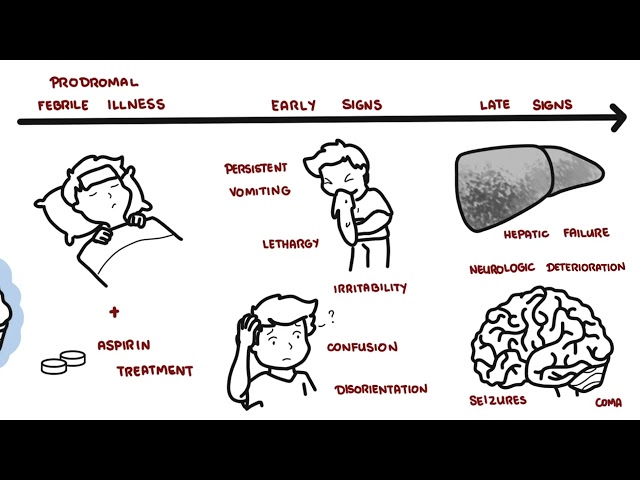
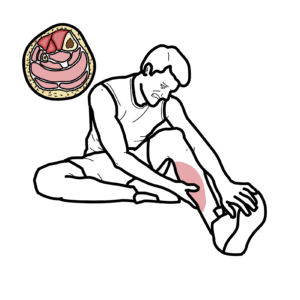
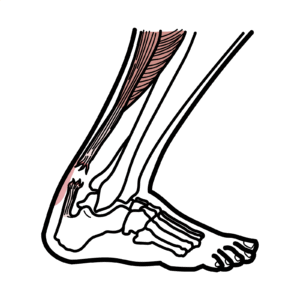
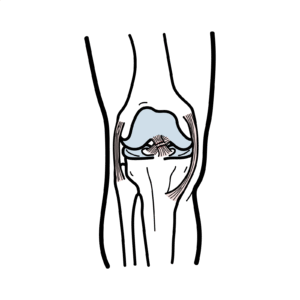
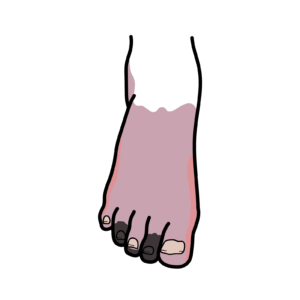
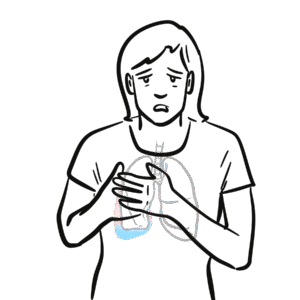
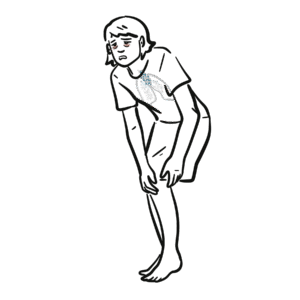
0:00 Patellofemoral syndrome, also known as runner's knee, is a common overuse 0:12 disorder of the knee 0:13 joint. 0:15 Patellofemoral syndrome is specifically diagnosed when there is no other 0:20 attributed pathology 0:21 such as a meniscuete, tendinitis, or bursitis. 0:26 It typically presents as anterior knee pain, behind the patella, and is 0:31 aggravated by activities 0:33 that involve loading the patellofemoral joint, such as during running or 0:38 jumping, and that 0:39 is why patellofemoral syndrome is also known as runner's knee. 0:46 Let's talk about some of the anatomy. 0:51 The knee joint is made up of the lower end of the femur, upper end of the tibia 0:55 , and 0:55 the patella. 1:02 The articular cartilage covers and protects the ends of the bones, where they 1:06 meet to form 1:07 the joint. 1:09 Within the joint themselves, there is another cartilage, the meniscus, which 1:14 helps cushion 1:15 the joints. 1:18 The knee joint is filled with a clear fluid, the synovial fluid, that acts as a 1:23 lubricant 1:23 to reduce friction within the joint. 1:28 There are also small, fluid-filled sacs called bursa, which cushions the joint 1:33 and help reduce 1:34 friction between the muscles and the other surrounding structures. 1:43 The patella is a bone. 1:45 It is the largest sesomoid bone in the human body. 1:50 It is located anterior to the knee joint, within the tendon of the quadriceps 1:57 muscles. 1:58 It provides an attachment point for both the quadriceps tendon and the patella 2:05 tendon, 2:06 or also known as the patella ligament. 2:09 The main function of the patella is to improve leverage for knee extension, so 2:15 during straightening 2:17 of the leg. 2:19 The patella moves along what is called the trochlear groove, during knee 2:23 extension and 2:24 flexion, moving up and down. 2:33 The mechanism of patellofemoral syndrome, there are a number of mechanisms, but 2:37 the main one 2:38 is an overuse injury, where there is excessive loading of the patellofemoral 2:45 joint. 2:45 Another mechanism for developing patellofemoral syndrome is if you have lower 2:51 limb malalignment. 2:53 If you have something called squinting patella, where the patella sits medially 2:59 , and if you 3:00 have femoral anti-version, as well as hyperpronation of the foot, this is an 3:11 example of what it 3:12 looks like when running. 3:17 Another mechanism is something called patella maltracking, so abnormalities 3:22 with tracking 3:23 of the patella. 3:24 Normally during knee flexion and knee extension, the patella travels within the 3:29 trochlear groove 3:30 and the intercondola notch of the fema. 3:34 The movement of the patella is dependent on the muscles, the tendon, and the 3:39 retinaculum 3:40 that surrounds it. 3:42 Any imbalance of these is most likely to cause the patella to track more later 3:49 ally, so during 3:50 episodes of loading, patellofemoral syndrome, or symptoms may arise as a result 3:56 . 3:57 The causes of patella tracking, or maltracking, are usually a result of 4:02 weakness or tightness 4:04 of muscle groups. 4:07 So this includes tightness of the vastus lateralis, rectus femoris, the 4:11 hamstring muscles, or the 4:13 iliotibial bang. 4:15 Alternatively, it could be due to weakness of the vastus medialis, allowing the 4:20 patella 4:21 to track more laterally. 4:28 Another mechanism of patellofemoral syndrome is due to issues with the Q angle, 4:33 so the 4:34 Q angle refers to the angle at the junction between two lines drawn from the 4:40 anterior 4:40 superior iliac spine to the middle of the patella, and then another line drawn 4:45 to the 4:45 same point from the tibial tubercle, or tibial tuberosity. 4:51 Now this normal angle is less than 20 degrees. 4:58 A greater than normal angle is associated with patella maltracking, so moving 5:04 laterally, 5:05 for example, and females tend to have a greater Q angle than of men, which will 5:12 also predispose 5:13 them to having patella maltracking and thus, patellofemoral syndrome. 5:23 The clinical presentation of patellofemoral syndrome is really patellofemoral 5:28 pain, which 5:29 is vague, aching pain over the anterior aspect of the knee. 5:34 It is aggravated by activity, especially distance running, squatting, lunging, 5:40 going up or down 5:42 stairs or sitting for long periods, and this is again in part due to the patell 5:49 a maltracking. 5:51 The patient may describe a clicking or grating behind the patella on knee 5:56 movement. 5:57 The knee may give way due to pain and quadriceps inhibition. 6:06 On clinical examination, there can be tenderness of the medial or lateral 6:11 facets of the patella. 6:12 There can be a small effusion, a bit of fluid within the knee joint, crepitus, 6:18 and stiffness 6:19 of patella movement as well as wasting of the vastus medialis. 6:27 It's important to exclude other diagnoses before diagnosing anyone with patell 6:32 ofemoral 6:33 syndrome. 6:35 Differentials for anterior knee pain to consider include ligamentus injuries, 6:40 meniscal injuries, 6:43 melanitis of the patella or quadriceps tendon, bursitis, and iliotibial band 6:55 syndrome. 6:57 Treatment of patellofemoral syndrome primarily aims to attempt to correct any 7:02 abnormal biomechanics, 7:03 so the malalignment we've discussed that contributes to patellofemoral syndrome 7:09 . 7:09 So manual treatment and stretching of tight muscles, for example, which may 7:13 contribute 7:14 to patellofemoral tracking, and these include tight iliotibial band, hamstring, 7:19 gastrocnemus 7:21 or the quadriceps, patella taping to correct any malposition or tilt of the p 7:27 atella to 7:28 reduce the pain. 7:31 Strengthening the muscles, for example, the gluteus medius or vastus medialis, 7:39 orthotics 7:40 to correct hyperpronation, which if you remember is a contributor to patellofem 7:45 oral syndrome. 7:47 Modifications of training regime to avoid overuse injury, surgery is typically 7:54 not required. 8:00 So in summary, patellofemoral syndrome is also known as run as knee, and is due 8:05 to an overuse 8:06 injury. 8:09 There are many contributing factors including malalignment, such as hyperpron 8:15 ation, as well 8:16 as abnormalities in patella tracking. 8:22 Treatment is generally conservative with strengthening exercises and stretching 8:27 . 8:28 Tis typically not required.